Healing with Foam: Effective Dressings for Burn Management

Why Foam Dressing for Burns Matters in Modern Wound Care
Foam dressing for burns offers a modern approach to wound management that balances effective healing with patient comfort. In short, foam dressings absorb wound fluid, maintain a moist healing environment, reduce pain during dressing changes, and can stay in place for several days, making them an excellent choice for partial-thickness burns.
Key Benefits of Foam Dressings for Burns:
- Superior exudate management - Absorbs fluid while keeping the wound bed moist
- Reduced pain - Gentle adhesion and cushioning minimize discomfort
- Fewer dressing changes - Can typically stay in place for up to 7 days
- Lower infection risk - Antimicrobial versions (especially silver-containing) help control bacteria
- Protection of surrounding skin - Prevents maceration and irritation
Burn injuries are common, and traditional care often involves painful, daily dressing changes with gauze. Foam dressings represent a significant advancement. The challenge with burns is their dynamic nature; they can deepen without proper care and produce varying amounts of fluid (exudate) that needs careful management. Too much moisture leads to skin breakdown (maceration), while too little slows healing.
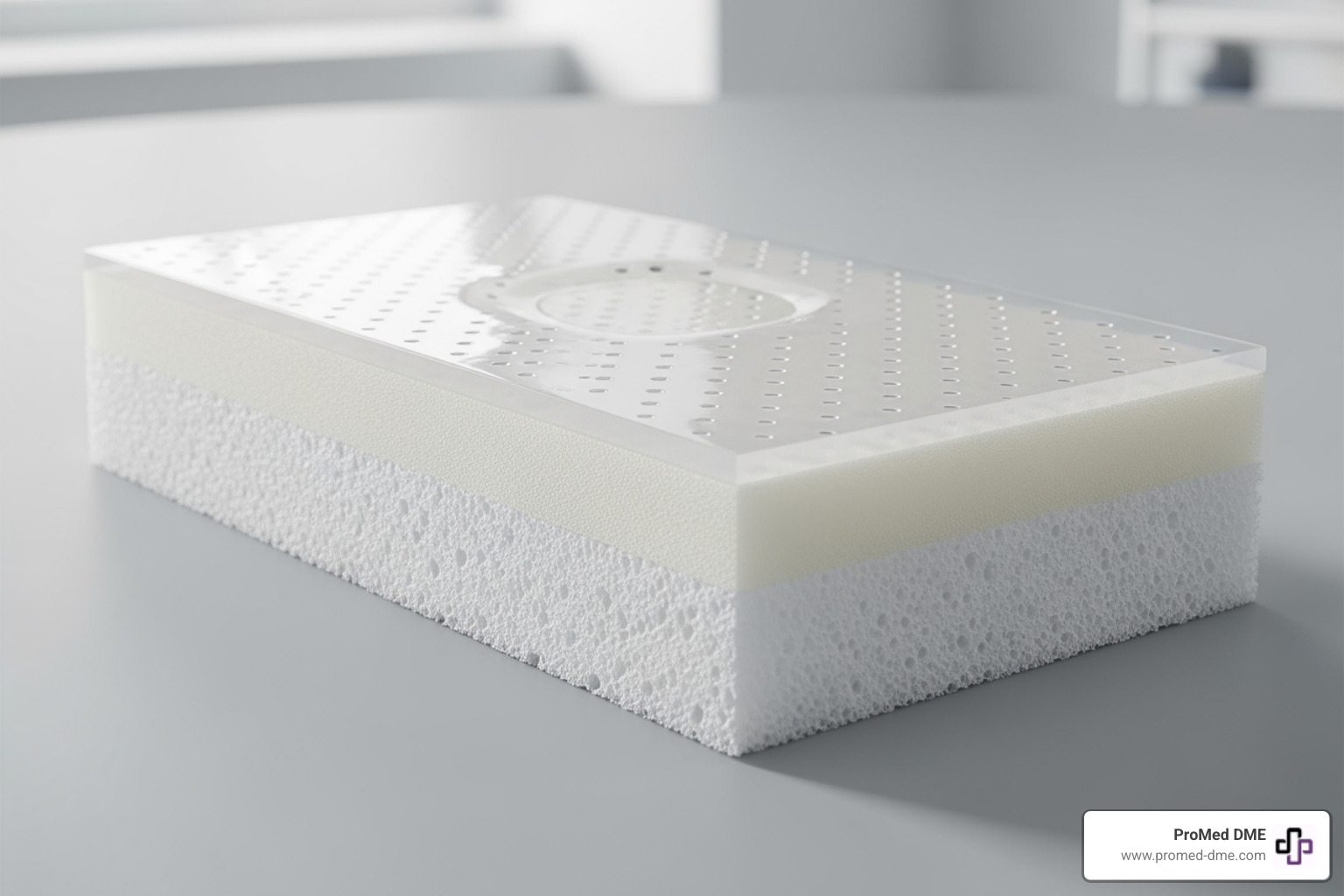
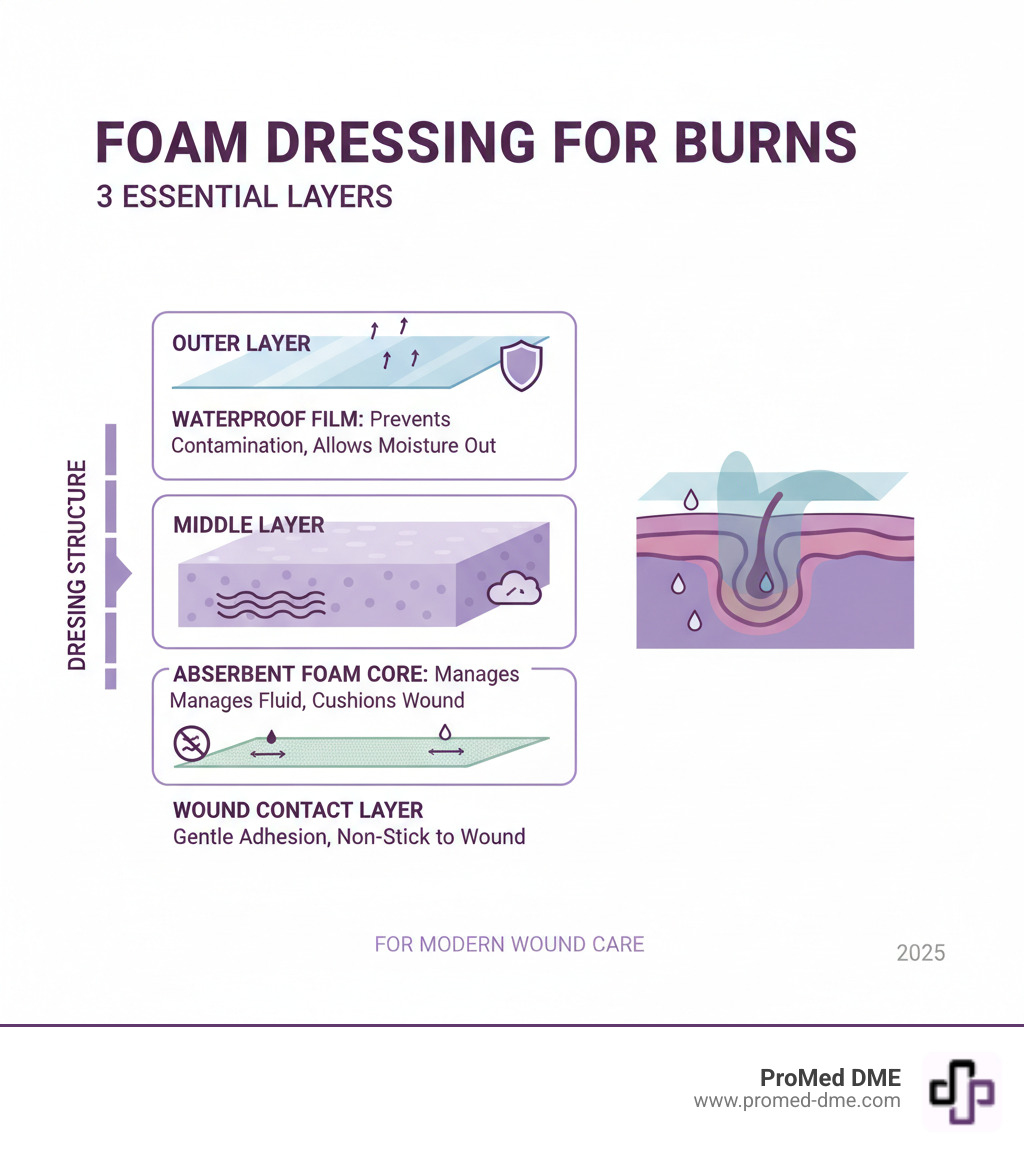
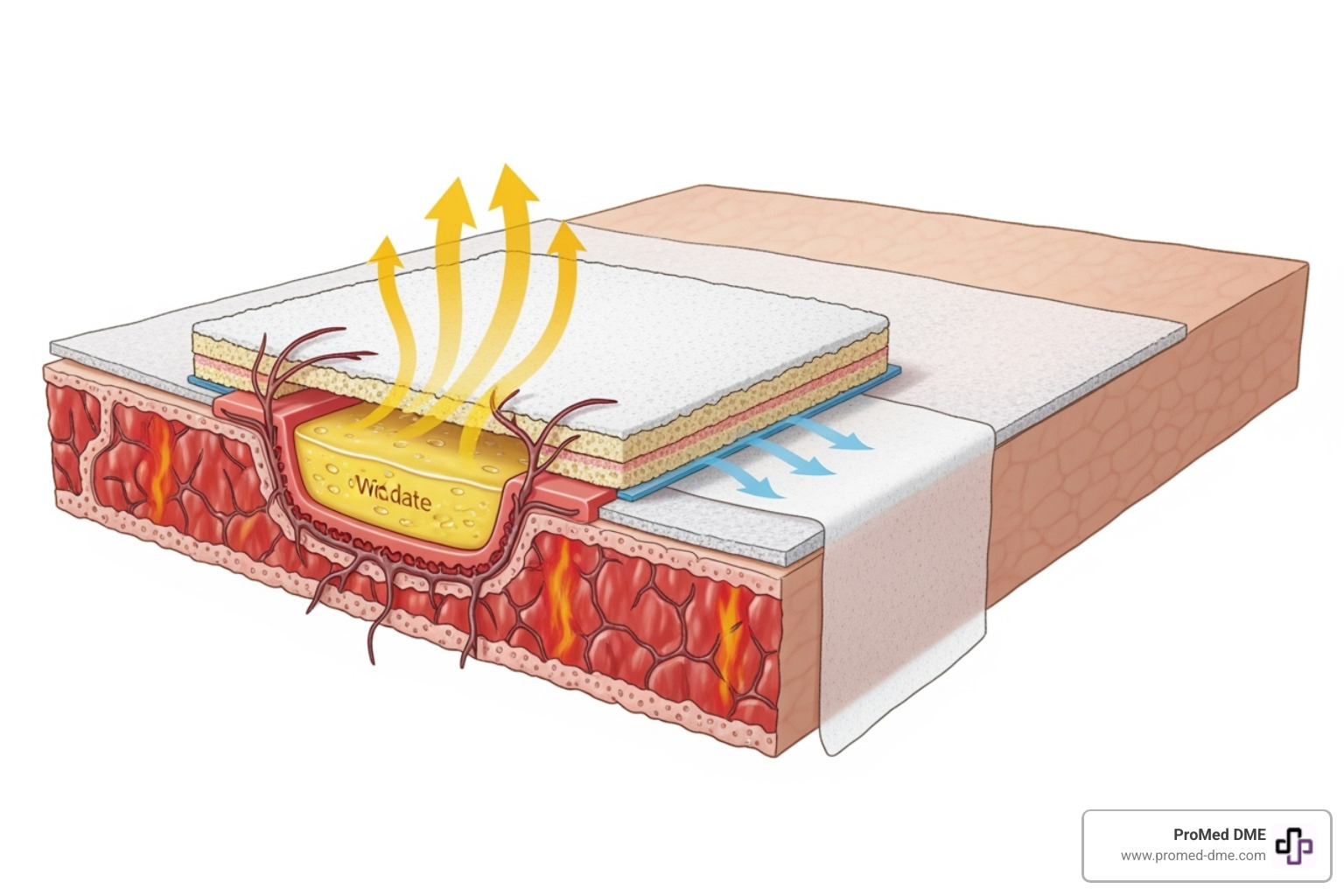
Foam dressings address these challenges with a unique structure: an absorbent foam core, a waterproof yet breathable outer layer, and a non-stick wound contact layer. Many also include antimicrobial agents like silver to reduce infection risk. Evidence shows they offer similar healing times to traditional methods but with significantly less pain and potentially lower infection rates.
Understanding Foam Dressings for Burn Care
When dealing with a burn, the right dressing can mean the difference between a comfortable healing process and a painful ordeal. Foam dressings for burns are a cornerstone of modern wound care because they address multiple challenges at once.
A foam dressing is a sophisticated moisture manager. Its absorbent core draws excess fluid (exudate) away from the wound while keeping the surface moist enough for optimal healing. This balance is crucial, as too much moisture leads to skin breakdown (maceration), while too little slows healing. The outer film is a waterproof, breathable shield against contaminants, while the foam itself provides thermal insulation and protective cushioning against bumps and pressure.
Types of foam dressing for burns
Foam dressings come in several configurations to match specific needs:
- Non-adhesive foam: Requires tape or a secondary dressing to secure. Ideal for fragile skin where adhesives could cause trauma.
- Adhesive bordered foam: Features a built-in adhesive frame for convenient, secure fixation on healthy skin around the wound.
- Foam with soft silicone technology: A leap forward in comfort, the silicone layer adheres gently to dry skin but won't stick to the moist wound bed, dramatically reducing pain during changes.
- Silver-containing foam: Adds antimicrobial power. Silver ions embedded in the foam help control bacteria and reduce infection risk, making them invaluable for contaminated burns.
- Ibuprofen-containing foam: An innovative option that combines wound management with localized pain relief by releasing a low dose of ibuprofen directly into the wound.
The Role of Silver and Other Antimicrobials
Infection is a major threat to burn healing. Silver has been used in wound care for centuries because it works. When a foam dressing for burns contains silver, it releases antimicrobial silver ions upon contact with wound fluid.
The mechanism of silver ions is a triple threat: they disrupt bacterial cell walls, interfere with metabolism, and prevent reproduction. This broad-spectrum antimicrobial activity is effective against a wide range of organisms, making silver dressings valuable for reducing bioburden (the number of bacteria) in contaminated or high-risk wounds.
By keeping bacteria in check, silver dressings promote a cleaner healing environment, leading to better infection prevention and a smoother recovery. For more detailed information, this research on silver in burn care provides evidence-based insights.
How Foam Dressing for Burns Compares to Other Treatments
For years, silver sulfadiazine (SSD) cream with gauze was the standard for partial-thickness burns. But foam dressing for burns offers a modern, more comfortable alternative. Studies show that silver foam dressings perform just as well as SSD with gauze in terms of healing time comparison, with some evidence suggesting slightly faster healing in the early stages.
Where foam dressings truly excel is in reducing pain. Research consistently shows that patients using foam dressings report significantly lower pain score differences, especially during the difficult first week. The infection rate data also favors foam dressings, with one study finding that only 5.9% of patients using silver foam had positive bacterial cultures by Day 28, compared to 15.4% in the SSD group.
Foam vs. Traditional Silver Sulfadiazine (SSD) with Gauze
Here is a head-to-head comparison of foam dressing for burns and the traditional SSD with gauze approach:
| Feature | Foam Dressings (e.g., Silver Foam) | Traditional SSD with Gauze |
|---|---|---|
| Change Frequency | Less frequent (typically every 2-7 days) | Daily changes |
| Pain on Removal | Significantly reduced due to gentle adhesion | Often painful as gauze can stick to the wound bed |
| Exudate Handling | Excellent absorption, prevents maceration | Can become saturated, less effective at preventing maceration |
| Healing Time | Similar to SSD, some studies show slightly faster early healing | Similar to foam, but can be hindered by pseudoeschar |
| Cost-Effectiveness | Potentially lower overall cost due to fewer changes and less nursing time | Higher overall cost due to daily changes and materials |
Beyond the points in the table, SSD can create a thick, whitish layer (pseudoeschar) that obscures the wound and can slow healing. Foam dressings avoid this issue. For patient comfort, there's no contest. The gentle removal and cushioning effect of foam provide a level of comfort that traditional gauze cannot match.
Foam vs. Other Advanced Dressings
Foam is an excellent choice, but it's not the only advanced dressing. Matching the dressing to the wound is key.
- Hydrocolloids: Best for low to moderate drainage. They form a gel to keep the wound moist but can be overwhelmed by heavy fluid.
- Alginates: Made from seaweed, these are absorption powerhouses for heavily draining burns. They require a secondary dressing.
- Hydrogels: Mostly water or glycerin, they are ideal for rehydrating dry or crusty burns but are not suitable for draining wounds.
- Transparent films: Thin, waterproof sheets for very superficial burns with no drainage. They allow for easy monitoring but offer no absorption.
So, when should you choose foam? Foam dressings for burns are the top choice for partial-thickness burns with moderate to heavy fluid, especially when pain management and cushioning are priorities. They perfectly balance moisture management, creating the "Goldilocks zone" for burn care.
Key Benefits of Using Foam Dressings
Foam dressing for burns actively supports healing while making the experience more bearable. They offer a compelling set of benefits that go far beyond simply covering a wound.
One of the most practical advantages is fewer dressing changes. Unlike traditional daily changes, foam dressings can often stay in place for up to a week. This convenience also leads to reduced treatment costs due to less nursing time and fewer supplies. Most importantly, it means better pain management during changes. Modern foam dressings with gentle adhesion technologies lift away cleanly without tearing at new tissue, changing a painful ordeal into a manageable process. They also protect the surrounding skin by wicking away fluid and preventing breakdown (maceration).
Enhancing Patient Comfort and Reducing Pain
If there's one area where foam dressing for burns excels, it's comfort. The secret lies in gentle adhesion, often using soft silicone that sticks to dry skin but not the moist wound bed. This non-adherent wound contact layer means less trauma on removal. The cushioning effect of the foam core also protects the sensitive burn area from bumps and pressure. Together, these features lead to less pain, less anxiety, and a significant reduction in the burning sensation often associated with burn wounds.
Managing Exudate and Preventing Maceration
Balancing moisture is a key challenge in burn care. Foam dressing for burns excels at this through high absorbency. The foam core wicks fluid away from the wound, preventing it from pooling and causing maceration. Many advanced foams also have an adaptive moisture vapor transmission rate (MVTR), where the outer film allows more moisture to escape when the wound is wet and less when it's dry.
This technology helps in maintaining a balanced moist environment, which is proven to speed up healing. By effectively managing fluid, foam dressings also excel at protecting periwound skin. The dressing is typically applied to overlap the wound edges, creating a protective zone that prevents fluid from irritating the delicate surrounding skin.
A Practical Guide to Application and Selection
Properly applying and selecting a foam dressing for burns is key to effective healing. While your healthcare provider will guide you, understanding the basics can help you feel more involved in your care.

Before applying any dressing, wound bed preparation is essential. Gently clean the burn with sterile saline or water. Your provider may need to perform debridement (removing dead tissue) for deeper burns. For sizing, the dressing should cover the burn and extend 1-2 cm onto healthy skin to protect it from fluid. Securing the dressing is done with the built-in adhesive border or with medical tape or a conforming bandage for non-adhesive types.
Application and Changing Protocols
Always follow your provider's instructions. Here are the general steps for applying and changing a foam dressing for burns:
- Preparation: Gently clean the burn and pat the surrounding skin dry.
- Application: Select and trim a dressing to size, ensuring a 1-2 cm overlap. Peel off the backing, place the foam over the burn, and smooth the edges. Secure with tape if non-adhesive.
- Frequency of Changes: Foam dressings can stay on for up to 7 days, depending on the amount of fluid. This means fewer painful changes and less disruption to healing.
- When to Change: Change the dressing if it becomes saturated with fluid, starts to lift or peel, or if you see signs of infection (increased pain, redness, swelling, odor).
- Removal Technique: Gently lift a corner, moistening with saline if it sticks. Peel back slowly while supporting the skin. Observe the wound for any changes.
For more general information, the MedlinePlus Health Information on burns is an excellent resource.
Indications and Contraindications for Foam Dressings
Foam dressings are ideal for partial-thickness burns with moderate to heavy fluid. Antimicrobial versions are valuable for infected burns or those at high risk of infection. The cushioning is also a major advantage for painful burns.
However, they are not for every situation. Contraindications include:
- Third-degree (full-thickness) burns, which require surgical treatment.
- Very dry burns with minimal fluid (a hydrogel is better).
- Known allergies to dressing components (like silver).
Choosing the right foam dressing for burns
Select the right dressing by considering these factors:
- Burn Depth: Foam is best for partial-thickness burns, not superficial first-degree or full-thickness third-degree burns.
- Exudate Level: Match the foam's absorbency to the amount of fluid the burn is producing (light, moderate, or heavy).
- Signs of Infection: If you see redness, swelling, or pus, an antimicrobial silver foam is the better choice.
- Wound Location and Size: A flexible foam is needed for joints, while a large adhesive dressing may work for a flat area like the back.
At ProMed DME, our on-staff nurse can help you steer these options. We carry a wide range of supplies, work with most insurance, and offer free shipping to minimize your costs and worries.
Frequently Asked Questions about Foam Dressings for Burns
Here are answers to common questions about using foam dressing for burns to help you feel more confident in your care choices.
Can you use a foam dressing on a fresh burn?
Yes, but only after proper first aid. The absolute first step is to cool the burn under cool (not ice-cold) running water for at least 10-20 minutes. This stops the burning process and reduces tissue damage.
Once cooled, a foam dressing for burns is an excellent choice for a partial-thickness burn (one with blistering or broken skin). It protects the area, absorbs fluid, and creates an ideal healing environment. For minor, red burns without broken skin, a foam dressing is likely not needed.
Seek medical advice immediately for any burn that is large, deep, on the face, hands, feet, or joints, or if you are unsure of its severity. Burns can deepen in the first 48 hours, so a professional assessment is crucial.
How long can a foam dressing stay on a burn?
One of the biggest benefits of foam dressing for burns is that it can stay in place for up to 7 days, unlike daily gauze changes. This means fewer painful changes and less disruption to healing.
The actual wear time depends on the amount of fluid (exudate) the burn produces. A heavily draining burn may require a change every 1-3 days, while a burn with minimal fluid might last the full week.
Change the dressing if you see fluid reaching the edges, if it starts to lift or leak, or if you notice any signs of infection (increased pain, redness, swelling, or odor). Always follow the manufacturer's instructions for your specific product.
Do foam dressings help reduce scarring?
While no dressing can completely prevent scarring, a foam dressing for burns can significantly minimize it by creating optimal healing conditions.
- Moist Wound Healing: Foam dressings maintain the perfect moisture balance, allowing skin cells to migrate more efficiently. This leads to faster, calmer healing, which generally results in better-looking scars.
- Infection Prevention: By providing a protective barrier (and an antimicrobial shield, in the case of silver foams), these dressings prevent infection, a major cause of poor healing and increased scarring.
- Faster Healing: Burns that heal within 21 days are less likely to form significant scars. By promoting efficient, undisturbed healing, foam dressings help burns close faster.
After the wound has closed, post-healing care is critical. Keep the new skin moisturized and, most importantly, protect it from the sun. Use a high-SPF sunscreen on the healed area for up to two years to prevent darkening (hyperpigmentation) and help the scar mature smoothly.
Conclusion
Modern wound care has made burn recovery more comfortable and effective, with foam dressing for burns leading the way for partial-thickness injuries. These dressings excel at managing fluid, protecting surrounding skin, and providing cushioning. Their gentle adhesion technology transforms the patient experience, making dressing changes far less painful.
By allowing for fewer changes, reducing costs, and offering antimicrobial protection, foam dressings support faster healing and reduced pain. They represent a more advanced, patient-centered approach compared to many traditional methods.
At ProMed DME, we are committed to supporting your healing journey with top-quality wound care solutions. Managing a burn requires reliable products and expert guidance, which is why we have a dedicated nurse on staff to answer your questions.
We offer free shipping across the United States and work with most insurance plans to minimize your out-of-pocket costs. For any burn injury or wound care need, we're here to make the process as smooth as possible.
Ready to find the right wound care supplies? We're here to help you heal better.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.