All About Bladder Weakness: Causes, Symptoms & Management

Does bladder weakness have you feeling confined and frustrated, affecting your quality of life? You're not alone. Millions of people experience urinary incontinence, which is a medical term for bladder weakness. At ProMed DME, we understand just how much an unpredictable bladder can impact your everyday life, from limiting your activities to causing embarrassment or anxiety.
Bladder weakness is a common issue that can stem from various causes such as age, childbirth, medical conditions, or lifestyle factors. Often, it presents as a sudden urge to urinate or an inability to control urine flow, leading to leakage. While these symptoms can feel isolating and uncomfortable, know that solutions exist and there's no need to suffer in silence.
Here's a brief at-a-glance understanding of bladder weakness:
- Types of urinary incontinence: Stress, urge, overflow, and total.
- Common causes: Aging, pregnancy, childbirth, menopause, medical conditions, and certain lifestyle factors.
- Symptoms: Uncontrollable urine leakage, frequent urination, sudden urges to urinate.
- Management: Lifestyle changes, pelvic floor exercises, dietary adjustments, and incontinence products.
Through this guide, we'll explain bladder weakness in a way that's easy to understand. We'll explore what triggers it, dive into its symptoms and types, and most importantly, offer strategies to manage it effectively. With our help, you'll regain confidence, uplift your spirit, and restore your freedom. It's time to break free from bladder weakness and continue living life on your own terms.
Understanding Urinary Incontinence: The Medical Term for Bladder Weakness
What is Urinary Incontinence?
Urinary incontinence, also known as bladder weakness, is a common condition that affects many people, especially as they age. It's characterized by the loss of bladder control, which can range from minor leaks when you cough or sneeze to a strong, sudden urge to urinate that you can't control in time. It's essential to understand that urinary incontinence is a symptom, not a disease in itself. It signals that something in your urinary system is not working correctly.
At ProMed DME, we believe that understanding your body's signals is the first step towards regaining control, and we're here to guide you through this process.
The Urinary System: How it Works and What Can Go Wrong
The urinary system includes the kidneys, ureters, bladder, and urethra, all of which work together to remove waste from your body through urine. The kidneys filter waste from your blood to form urine, which then flows down the ureters into the bladder. When your bladder is full, a signal is sent to your brain, and you feel the urge to urinate. Urine then leaves the body through the urethra.
In bladder weakness, the urinary system's process is disrupted. The bladder may not empty completely, leading to overflow incontinence. In other cases, you may experience a sudden, intense urge to urinate, known as urge incontinence. Furthermore, the female urethra's short length simplifies catheter insertion but increases the risk of urinary tract infections (UTIs).
Temporary vs. Chronic Incontinence: The Differences
Incontinence can be temporary or chronic. Temporary incontinence can be due to factors such as a urinary tract infection or certain medications, and it usually resolves once the underlying cause is treated. Chronic incontinence, on the other hand, persists over time and may be caused by underlying conditions such as neurological disorders, diabetes, or physical impairments that prevent you from reaching the toilet in time.
In either case, it's crucial to seek medical advice if incontinence is frequent or affecting your quality of life. At ProMed DME, we understand that discussing incontinence can feel uncomfortable. However, we're committed to providing the highest quality medical supplies and knowledge to help you manage your health concerns with confidence.
In the next sections, we'll delve deeper into the causes, symptoms, and types of urinary incontinence, providing you with a comprehensive understanding of this condition. Together, we can navigate the challenges of bladder weakness and work towards improving your quality of life.
Causes of Bladder Weakness
Bladder weakness, or urinary incontinence, is the involuntary leakage of urine. Various factors can cause this condition, from aging and lifestyle habits to underlying health issues. Let's explore these causes in more detail.
Age, Pregnancy, Childbirth, and Menopause: How They Affect Bladder Control
Bladder control can be significantly influenced by natural life events.
Aging is a common factor. As we age, the muscles responsible for bladder control may weaken, causing involuntary leakage.
Pregnancy and childbirth can also affect bladder control. The weight of a growing fetus can put pressure on the bladder, leading to stress incontinence. Additionally, vaginal childbirth can weaken pelvic floor muscles and damage nerves that control the bladder.
Menopause is another significant factor. The decline in estrogen during menopause can lead to a weakening of the muscles that control the bladder and urethra, increasing the likelihood of incontinence.
Medical Conditions That Can Lead to Bladder Weakness
Certain medical conditions can directly impact bladder control. These include:
- Diabetes: High blood sugar levels can cause nerve damage, affecting the nerves that control the bladder.
- Neurological disorders: Stroke, Parkinson’s disease, multiple sclerosis, and Alzheimer’s disease can disrupt the nerve signals involved in bladder control, leading to incontinence.
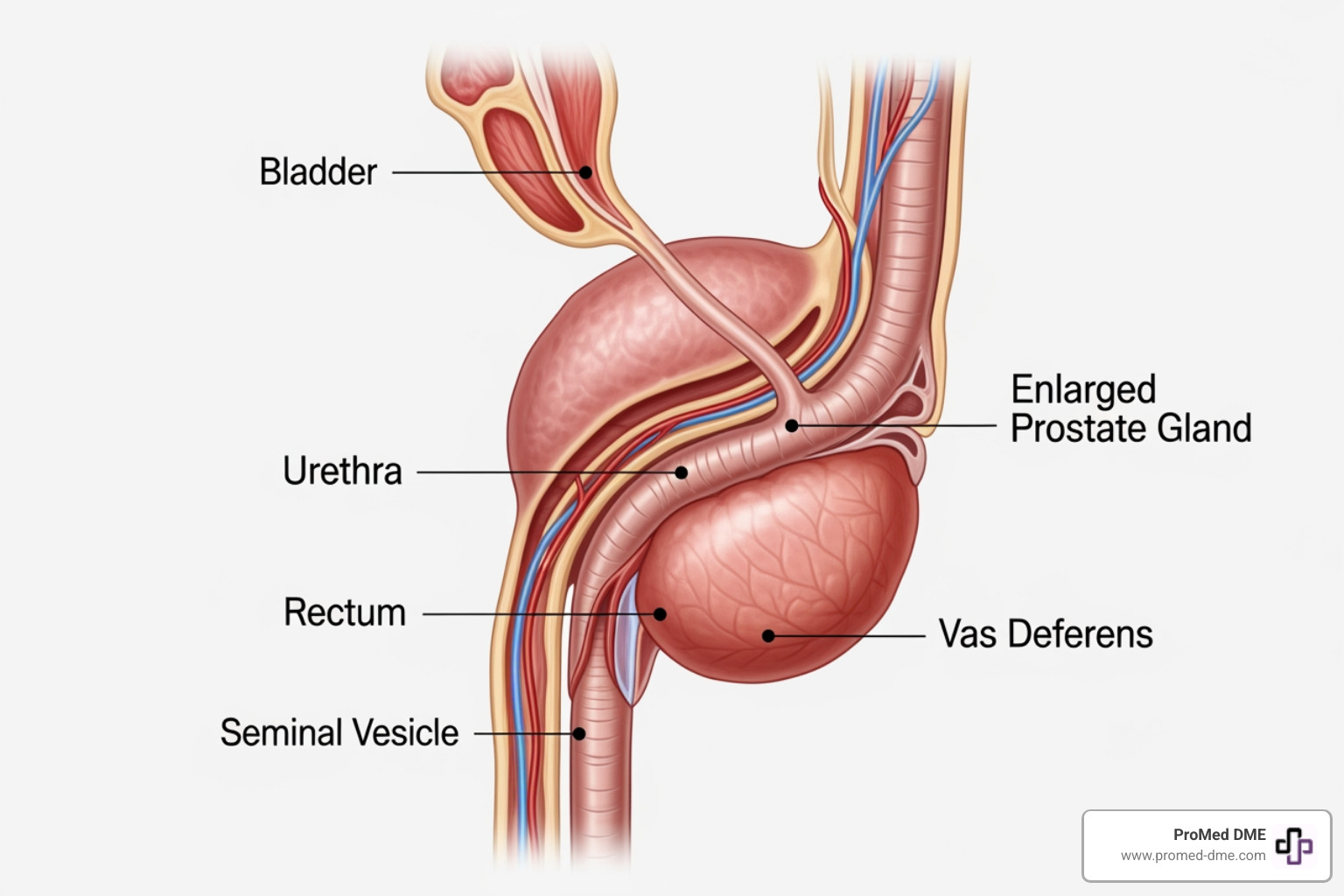
- Prostate problems in men: An enlarged prostate can block the flow of urine, leading to overflow incontinence. Prostate cancer treatments can also cause stress and urge incontinence.
Lifestyle Factors: Smoking, Obesity, and More
Lifestyle factors can also contribute to bladder weakness.
Smoking can cause chronic cough, which can lead to stress incontinence. Nicotine may also irritate the bladder muscles.
Obesity increases pressure on the bladder and surrounding muscles. This pressure can weaken the muscles over time and cause incontinence.
Poor diet and constipation: Regularly consuming foods and drinks that irritate the bladder may lead to urinary incontinence. Also, chronic constipation can weaken pelvic floor muscles, impacting bladder control.
At ProMed DME, we understand that bladder weakness can be a sensitive issue. We're committed to providing you with the necessary resources and products to manage this condition effectively. In the following sections, we'll explore the symptoms and types of urinary incontinence, as well as the available treatment options.
Symptoms and Types of Urinary Incontinence
Bladder weakness, or urinary incontinence, can manifest in various ways. The symptoms you experience can range from occasional leaks when you laugh or cough to a consistent dribble of urine. Understanding the different types of urinary incontinence can help you manage your symptoms effectively.
Stress Incontinence: Leaks When You Cough, Laugh, or Exercise
Stress incontinence is characterized by the leakage of urine when there's pressure exerted on your bladder. This pressure could be the result of everyday activities like coughing, laughing, exercising, or lifting heavy objects. The term "stress" in this context refers to physical strain or pressure, not emotional stress.
Urge Incontinence: Sudden and Strong Urge to Urinate
Urge incontinence, often associated with Overactive Bladder (OAB), is characterized by a sudden and intense urge to urinate, usually followed by an involuntary loss of urine. This urge can be so strong that you don't make it to the toilet in time. It can cause frequent urination, and you may find yourself waking up multiple times during the night to urinate.
Overflow Incontinence: Constant Dribbling of Urine
Overflow incontinence happens when you experience frequent or constant dribbling of urine due to a bladder that doesn't empty completely. You may feel as if you're unable to fully empty your bladder, leading to frequent small urinations or constant dribbling. This is more common in men with a history of prostate problems or surgery but can also occur in women due to conditions like diabetes or previous bladder surgeries.
Total Incontinence: Complete Loss of Bladder Control
Total incontinence is the most severe form of bladder weakness. It involves complete loss of bladder control, leading to continuous leakage of urine. This can be caused by a physical or mental impairment that keeps you from reaching the toilet in time.
If you're experiencing any of these symptoms, don't hesitate to seek medical advice. At ProMed DME, we offer a range of urology products that can help manage the symptoms of urinary incontinence, providing you with the freedom and confidence to live your life to the fullest.
Diagnosis and Treatment of Bladder Weakness
How is Bladder Weakness Diagnosed?
Diagnosing bladder weakness involves a few key steps. First, your healthcare provider will likely conduct a thorough medical history check and physical examination. This can help rule out other possible conditions and identify any risk factors you may have.
In addition, diagnostic testing for urinary incontinence includes urinalysis and urine culture, two procedures that check for the presence of substances that point to various conditions, including urinary tract infections (UTIs), which are a common cause of temporary incontinence. During a urine culture, the type of bacteria causing the infection is identified, a crucial step that guides the selection of the most effective antibiotic for treatment, if necessary.
Recognizing the symptoms is paramount. Timely recognition can lead to prompt diagnosis and treatment.
Non-Surgical Treatments: Lifestyle Changes, Pelvic Floor Exercises, and Bladder Training
Often, non-surgical treatments can effectively manage bladder weakness. These include lifestyle changes, like losing excess weight, quitting smoking, and cutting down on caffeine and alcohol.
A key component of non-surgical treatment is the practice of pelvic floor exercises, also known as Kegel exercises. These exercises are designed to strengthen the muscles that help hold urine in the bladder. Daily practice can improve their strength and hence, bladder control.
Bladder training is another effective strategy. This involves gradually increasing the intervals between using the bathroom, helping retrain your bladder to hold urine for longer periods.
At ProMed DME, we're here to support you with the right products and knowledge to manage your bladder weakness symptoms effectively.
Surgical Treatments: When are They Necessary?
In some cases, when non-surgical treatments aren't enough, surgical procedures might be recommended. These are generally reserved for severe cases, for instance, when a person is unable to pass urine, has kidney damage, frequent UTIs, or a lot of bleeding.
Options like Prostatic Urethral Lift (PUL) use tiny implants to lift and compress the prostate, reducing blockage. Another option is Water Vapor Thermal Therapy (WVTT), which uses steam to destroy prostate cells, causing the prostate to shrink.
More invasive surgeries, such as Transurethral Resection of the Prostate (TURP) and Simple Prostatectomy, are usually administered in severe cases.
Each treatment option has its pros and cons, and it's crucial to discuss these with your healthcare provider. We're here to guide you every step of the way, providing you with the right products and knowledge to manage your bladder weakness symptoms effectively. You're not alone in this journey, and we're committed to helping you navigate your health with confidence.
Managing Bladder Weakness: Practical Tips and Strategies
Living with bladder weakness doesn't mean giving up on a comfortable, fulfilling life. By incorporating a few simple changes into your daily routine, you can greatly improve your urinary incontinence symptoms. Let's explore some practical strategies that can help manage bladder weakness.
Pelvic Floor Exercises: How to Do Them and Why They Help
Pelvic floor exercises, also known as Kegel exercises, are a powerful tool in combating bladder weakness. These exercises serve to strengthen the muscles that hold urine in the bladder. When done regularly, they can help prevent urine leaks when you sneeze, laugh, cough, or have a sudden urge to urinate.
To do pelvic floor exercises correctly, you need to imagine that you're trying to stop the flow of urine or hold in a fart. This squeezing action engages the pelvic floor muscles. It's important to do these exercises daily and to remember to breathe normally while doing them. It may take up to three months to see benefits, but consistency is key.
Keep in mind that if you're a smoker, quitting can also improve your symptoms. Coughing from smoking can strain your pelvic floor muscles, exacerbating bladder weakness.
Dietary Adjustments: What to Eat and Drink to Improve Bladder Control
What you eat and drink can significantly affect bladder weakness. Certain foods and drinks can irritate the bladder, making incontinence worse. Caffeine is one such irritant, so consider switching to decaffeinated coffee or cutting down on other caffeine sources like tea, fizzy drinks, and chocolate.
Alcohol is another diuretic that makes you urinate more frequently, thus it's advisable to reduce your intake. Spicy and acidic foods, such as curries and citrus fruits, can also irritate the bladder.
On the other hand, drinking plenty of water can help with urinary retention. It might seem counterintuitive, but limiting fluid intake can actually worsen incontinence by reducing your bladder's capacity. Aim for 6 to 8 glasses of fluid per day unless advised otherwise by your doctor.
Incontinence Products: How They Can Help Manage Symptoms
While lifestyle adjustments can greatly improve bladder control, incontinence products can provide extra security and peace of mind. At ProMed DME, we offer a range of urology products designed to help you manage bladder weakness.
From incontinence pads and underwear to catheters, these products provide a practical solution for managing symptoms. They are designed to provide comfort, alleviate distress, and prevent complications such as urinary infections and kidney damage caused by urinary retention.
In the context of an enlarged prostate obstructing the urethra, for example, a catheter can provide immediate relief from urinary symptoms. It’s a temporary solution that can significantly improve quality of life while you and your healthcare provider work on a long-term treatment plan.
Managing bladder weakness is a journey, and we're here to support you every step of the way. Reach out to our team at ProMed DME for personalized advice and recommendations.

In the next section, we'll wrap up our comprehensive guide on bladder weakness. We'll remind you that while bladder weakness can be a challenge, it doesn't define you or your ability to lead a fulfilling life.
Conclusion: Living with Bladder Weakness and Seeking Help
Living with bladder weakness can be a challenging journey, but it doesn't have to limit your quality of life. It's crucial to remember that bladder weakness is a common condition that affects many people, especially older adults and women who have given birth or gone through menopause.
There are many strategies and treatments available to manage bladder weakness effectively. From simple lifestyle changes like pelvic floor exercises, to medical interventions such as urinary catheterization, there's a wide range of approaches to suit your specific needs and lifestyle.
Remember that being proactive in your healthcare is essential. Regularly practicing pelvic floor exercises can strengthen the muscles that control urination and help prevent urine leakage. Paying attention to your diet and hydration levels, avoiding irritants like caffeine and alcohol, and maintaining a healthy weight can also contribute significantly to managing bladder weakness.
In terms of medical management, urinary catheterization can be a necessary intervention. But with the right products, proper techniques, and a supportive healthcare team, it doesn't have to disrupt your life. As highlighted by ProMed DME, with the right support, you can continue to live a comfortable, fulfilling life.
It's also crucial to be aware of the signs of potential complications, such as Catheter-Associated Urinary Tract Infections (CAUTIs). Recognizing symptoms and seeking treatment promptly can prevent further complications and ensure your health and comfort.
Lastly, remember that you're not alone in this journey. Reach out to your healthcare provider or our team at ProMed DME for any further questions or concerns. We are here to support you every step of the way, ensuring you receive the best care and supplies for your needs.
Living with bladder weakness can be a challenge, but with the right information, tools, and support, you can effectively manage this condition and continue to lead a fulfilling life. To learn more about the products and services we offer to help manage bladder weakness, check out our urology page or contact us directly for personalized advice and recommendations.
Bladder weakness doesn't define you, and with the right support, you can manage this condition effectively. Here's to your health and wellbeing!

Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.