Enlarged Prostate and Catheters: What You Need to Know
Understanding Why a Catheter for Enlarged Prostate May Be Necessary
A catheter for enlarged prostate is a medical device used to drain urine when benign prostatic hyperplasia (BPH) causes a blockage. Many men with an enlarged prostate wonder when—and why—they might need one.
Quick Answer: When You Might Need a Catheter for BPH:
- Acute urinary retention - A sudden inability to urinate (a medical emergency)
- Before treatment - To drain the bladder for tests or surgery
- After BPH procedures - Temporary use during healing (e.g., 3-4 days for Rezūm)
- Chronic retention - When other treatments are not sufficient
You're not alone—about 50% of men have BPH by age 50, and most have it by age 80. As Bruce Gold shared with Cedars-Sinai after using a catheter for three months before finding a better treatment: "This procedure was a godsend. I'm back to where I was over 20 years ago."
The good news is that understanding your options, from catheters to modern treatments, empowers you to make informed choices. Many newer procedures have shorter catheter times or avoid them entirely. This guide will cover when a catheter is necessary, what to expect, and how treatments are reducing the need for long-term use.

Catheter for enlarged prostate vocab explained:
Understanding BPH and Its Impact on Urination
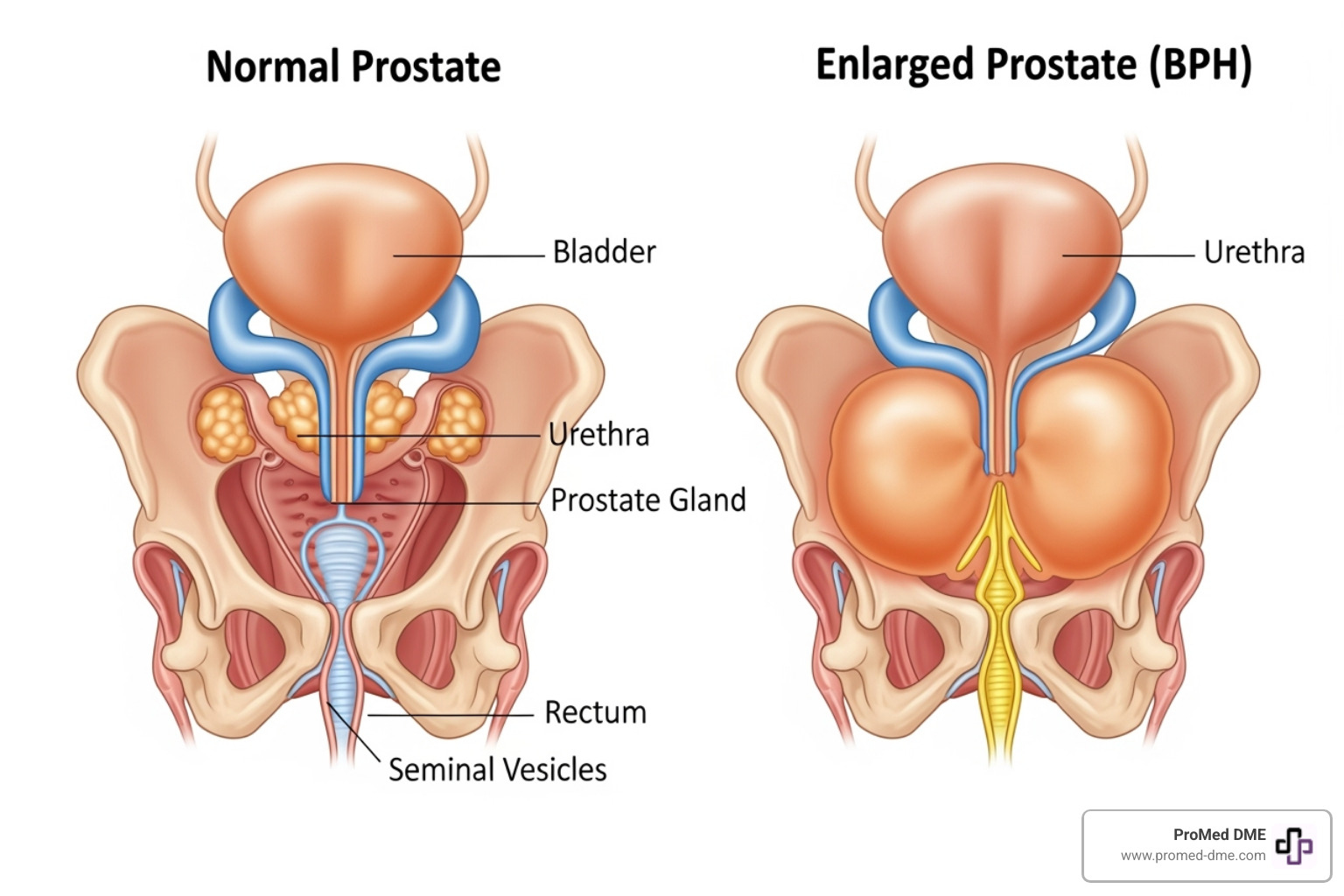
Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland. While not cancer, this common condition can significantly affect your daily life. The prostate wraps around the urethra (the tube that carries urine out of the body), and as it enlarges, it squeezes the urethra, restricting urine flow.
This compression causes Lower Urinary Tract Symptoms (LUTS), such as a weak or slow urine stream, frequent urination, waking at night to urinate (nocturia), and a feeling of incomplete bladder emptying. While a minor annoyance for some, these symptoms can be life-changing for others, affecting sleep, work, and social activities.
BPH is very common: about 50% of men have it by age 50, and most experience it by age 80. You are not alone.
Signs You Should Seek Medical Attention
While some urinary changes are normal with age, see your doctor for these warning signs:
- Urgency: A sudden, overwhelming need to urinate.
- Straining to urinate: Difficulty starting or maintaining a stream.
- Dribbling: Leaking after you think you've finished.
- Blood in your urine: Always requires a medical evaluation.
- Inability to urinate: Known as acute urinary retention (AUR), this is a medical emergency requiring immediate attention. This is a common reason a catheter for enlarged prostate is needed.
Ignoring these symptoms is risky. Untreated BPH can lead to urinary tract infections, bladder stones, or even bladder and kidney damage. Early treatment prevents these complications and improves quality of life. If you have these symptoms, contact your healthcare provider to discuss your options, which may include temporary use of a catheter for enlarged prostate. For more on how catheters work, Healthline's guide to urinary catheters is a helpful resource.
The Role of a Catheter for Enlarged Prostate
When BPH severely blocks the urethra, a catheter for enlarged prostate acts as a lifeline, creating a detour for urine to exit the bladder. It's essential in several situations:
- Acute Urinary Retention (AUR): A painful and sudden inability to urinate, which is a medical emergency. A catheter provides immediate relief by draining the bladder.
- Pre-surgical bladder drainage: An empty bladder provides a clearer view and safer environment for diagnostic tests or surgery.
- Post-procedure healing: After BPH procedures, a catheter allows the urethra to heal from swelling by ensuring urine can drain freely.
Two common types are the Foley catheter, which has a straight tip, and the Coudé catheter, which has a curved tip designed to steer around an enlarged prostate. Your doctor will select the best type for your anatomy.
While vital, catheters have risks. Catheter-Associated Urinary Tract Infections (CAUTIs) can occur as the catheter provides a pathway for bacteria. There's also a risk of urethral trauma during insertion, especially with an enlarged prostate. As medical literature notes, catheter placement can be challenging and poses risks of trauma and infection in men with obstructive conditions.
Why a Catheter Might Be Needed Before Treatment
In cases of acute urinary retention, a catheter for enlarged prostate is essential to prevent bladder and kidney damage. Once the immediate crisis is resolved, the catheter serves other key purposes. It allows your healthcare team to monitor urine output and kidney function, stabilizing your condition.
This provides crucial time to perform diagnostic tests like an ultrasound or cystoscopy to assess the prostate and plan the best course of action. With the emergency managed, you can discuss treatment options without pressure. The catheter may remain temporarily to see if medication can improve the situation, buying time to make the right decision.
Understanding the Risks and Discomforts of Catheterization
Living with a catheter can be challenging, and it's normal to feel apprehensive. Common issues include:
- Bladder spasms: Sudden, intense cramps as the bladder tries to empty, which can be uncomfortable and cause leakage.
- Leakage: Urine may escape around the catheter due to spasms, irritation, or incorrect sizing.
- Discomfort: A persistent feeling of pressure or irritation at the insertion site is common.
- Infection risk (CAUTI): Watch for fever, chills, cloudy or foul-smelling urine, or increased pain, and contact your provider immediately if these occur.
- Mobility challenges: Managing tubing and a drainage bag can feel awkward and restrictive.
- Psychological impact: It's valid to feel embarrassment, anxiety, or a loss of independence. As one medical source honestly acknowledges, potential challenges include "discomfort, inconvenience, embarrassment, and, although rare, trauma to the urethra and infection."
These challenges are often temporary. Your healthcare team and ProMed DME are here to help with pain relief, proper care techniques, and strategies to make daily life easier.
BPH Treatments and Post-Procedure Catheter Use
BPH treatment has advanced significantly, with options ranging from traditional surgery to innovative, minimally invasive procedures. Many newer treatments offer faster recovery and shorter catheter times—or none at all. Each approach has a different recovery timeline and catheter requirement.
| Treatment Type | Procedure Type | Recovery | Typical Catheter Duration | Sexual Side Effects (risk) |
|---|---|---|---|---|
| Traditional Surgery (TURP) | Transurethral Resection of the Prostate | More invasive, hospital stay | Up to 2 weeks | Ejaculatory dysfunction (common), Erectile dysfunction (possible) |
| Rezūm™ Water Vapor Therapy | Minimally Invasive, Water Vapor Ablation | Outpatient, quick return to activity | 3-4 days | Minimal impact on erectile/ejaculatory function |
| Prostate Artery Embolization (PAE) | Minimally Invasive, Interventional Radiology | Outpatient, minimal recovery | Rarely needed, if so, very short | Very low risk |
| Optilume® BPH Catheter System | Minimally Invasive, Drug-Coated Balloon | Outpatient/in-office, quick recovery | Minimal catheter time | No impact on sexual function |
| UroLift System | Minimally Invasive, Implants | Outpatient, quick return to activity | Rarely needed (if temporary, short) | Preserves sexual function |
Traditional surgery like TURP (Transurethral Resection of the Prostate) has been the gold standard for decades. While effective, it typically requires a hospital stay and up to two weeks with a catheter as your body heals. Minimally Invasive Procedures (MIPS) have changed the game, offering effective relief with much shorter recovery times. Interventional radiology techniques like PAE provide yet another avenue, often with the least amount of catheter time needed.
Rezūm™ Water Vapor Therapy and Recovery
Rezūm therapy uses controlled steam to eliminate excess prostate tissue blocking urine flow. During this minimally invasive procedure, water vapor is delivered into the prostate, causing obstructive cells to break down. Your body then naturally absorbs the treated tissue over several weeks, clearing the urinary path.
Post-procedure swelling is normal and a sign the treatment is working, but it can make urination difficult temporarily. For this reason, most men need a catheter for enlarged prostate for an average of 3-4 days. Your doctor will remove it once the swelling subsides. Home recovery involves keeping the catheter clean, staying hydrated, and managing pain as directed. Our nurse at ProMed DME can guide you through proper catheter care. For more details, visit Rezūm's patient resources.
Prostate Artery Embolization (PAE)
Prostate Artery Embolization (PAE) shrinks the prostate by cutting off its blood supply. An interventional radiologist guides a microcatheter to the prostate arteries and releases tiny beads to block them. Deprived of blood, the prostate tissue gradually shrinks.
A key benefit of PAE is the minimal need for post-procedure catheterization. Since the urethra isn't directly treated, there is less swelling. Many patients go home the same day without a catheter, or with one that is removed within hours. The Cedars-Sinai article calls PAE "life-changing," highlighting its nonsurgical, low-risk nature. Minimal recovery and catheter time make PAE an attractive option.
Why a catheter for enlarged prostate is common after treatment
Most BPH treatments require a temporary catheter because of the body's natural healing response: inflammation. Any treatment—whether using heat, steam, or surgery—causes temporary swelling in and around the prostate and urethra. This swelling can make urination difficult right after the procedure.
A catheter for enlarged prostate acts as a temporary ally, keeping the urinary path open while the swelling subsides. It ensures the bladder empties completely without straining, allowing the urethra to heal properly. This also prevents complications like acute urinary retention or bladder damage. While not ideal, a temporary catheter is often the smartest way to ensure a smooth recovery and the best long-term results.
Innovations in BPH and Catheter Technology
The landscape of BPH and catheter technology is rapidly evolving, offering less invasive treatments, faster recoveries, and a more comfortable catheter experience.
Innovations include:
- Visually-guided catheterization: This technology allows doctors to see inside the urethra during insertion, reducing the risk of trauma and improving precision compared to traditional "blind" insertion.
- The Optilume® BPH Catheter System: A breakthrough that combines mechanical opening of the urethra with targeted medication delivery.
- Drug-coated balloons: These devices widen the urethra while delivering medication to prevent tissue from re-blocking the urinary path.
These smart, targeted approaches are showing great promise.
New Catheter-Based Treatments for BPH
Catheter-based treatments offer a middle ground between daily medications and major surgery. The Optilume® BPH Catheter System is a leading example. In an outpatient procedure, a specialized catheter with a drug-coated balloon is used. When inflated, the balloon mechanically widens the urethra while releasing paclitaxel, a drug that prevents the prostate tissue from re-blocking the channel. This procedure offers minimal post-procedure catheter time, can often be done without general anesthesia, and preserves sexual function. Learn more from Laborie.
Another innovation is the Schelin Catheter®, which has an extra channel for delivering medication like local anesthesia directly into the prostate. This can reduce pain during procedures like Rezūm, lessen bleeding during TURP, and sometimes avoid the need for general anesthesia. Details are on the Schelin Catheter website. These in-office treatments offer a life-changing alternative for many men, avoiding hospital stays and preserving sexual function.
Advancements for Difficult Catheterizations
Inserting a catheter for enlarged prostate can be difficult due to the angles created by the prostate. As medical literature notes, this is a common challenge. Fortunately, advances are making catheterization safer and more manageable:
- Coudé-tip catheters: These have a curved tip that helps steer the angle of an enlarged prostate more easily than a standard straight-tip catheter.
- Smaller silicone catheters (12-14 French): Their flexibility can help them pass through narrowed areas.
- Visually-guided devices: These tools use tiny cameras, allowing providers to see inside the urethra during insertion, dramatically improving success rates and safety. One study showed a 100% success rate with visual guidance.
- Topical anesthetic gels: Proven to significantly reduce discomfort during insertion.
These techniques, combined, make modern catheter placement far more comfortable. For more details, see the article on Current Trends in the Management of Difficult Urinary Catheterizations. At ProMed DME, we stay current on these innovations to provide the most effective options. Our nurse can help you find the right catheter for your needs.
Frequently Asked Questions about BPH and Catheters
We know that facing BPH and the possibility of needing a catheter brings up a lot of questions. Let's walk through some of the concerns we hear most often.
How long will I need a catheter for my enlarged prostate?
The duration you'll need a catheter for enlarged prostate depends on your specific situation and treatment:
- Acute Urinary Retention: A catheter is used temporarily (from days to weeks) while your doctor determines the next steps.
- Minimally Invasive Procedures (e.g., Rezūm™): Catheter use is typically short, often just 3 to 4 days, to allow initial swelling to subside.
- Traditional Prostate Surgery (e.g., TURP): Healing takes longer, so expect to use a catheter for up to two weeks.
- Chronic Retention: In some cases where other treatments are not effective, a long-term catheter may be necessary to manage symptoms and maintain quality of life.
The final decision on timing rests with your physician, who will monitor your healing. Close communication with your healthcare team is key.
Is it painful to have a catheter inserted or removed?
It's natural to be nervous about catheter insertion and removal. Here’s what to expect:
- Insertion: A lubricating gel with a local anesthetic is used to numb the area and help the catheter glide smoothly. You will likely feel pressure, fullness, and a strong urge to urinate. While uncomfortable, the anesthetic gel and a gentle technique make it manageable for most men.
- Removal: This process is much quicker and easier. A nurse deflates the balloon holding the catheter in place and gently slides it out. You may feel a brief pressure or slight burning sensation.
After removal, it's normal to have some temporary burning during urination, which usually subsides within a day or two.
How do I care for a catheter at home?
Home catheter care becomes routine with practice. Our dedicated nurse at ProMed DME is available to help. Here are the key steps:
- Hand Hygiene: Always wash your hands with soap and water before and after touching your catheter or drainage bag to prevent infection.
- Clean the Insertion Site: At least twice daily, gently clean the skin where the catheter enters the body with mild soap and water.
- Keep Drainage Bag Low: The drainage bag must always be kept below the level of your bladder to prevent urine from flowing backward.
- Stay Hydrated: Drink plenty of fluids (mostly water) to help flush your system and reduce infection risk.
- Prevent Constipation: A high-fiber diet and adequate fluids can prevent straining, which puts pressure on the bladder.
- Secure the Tubing: Use a strap to secure the tubing to your thigh to prevent painful tugging or injury.
- Empty Drainage Bags Regularly: Empty leg bags when they are about half full (every 3-4 hours) and night bags each morning. Clean reusable bags daily as instructed.
- Watch for Warning Signs: Contact your doctor immediately for signs of infection or blockage, such as fever, chills, cloudy or foul-smelling urine, increased pain, significant leakage, or no urine drainage.
ProMed DME provides all the necessary supplies, from urinary catheters to drainage bags. Our team is here to support you.
Conclusion
Understanding your health is the first step to feeling in control. While dealing with an enlarged prostate and the potential need for a catheter for enlarged prostate can be overwhelming, there are many reasons to be optimistic.
This guide has covered why a catheter might be needed and explored the full spectrum of treatments, from traditional surgery to minimally invasive options like Rezūm, PAE, and the Optilume system. While a catheter for enlarged prostate may be part of your journey, it is often temporary. Modern treatments are significantly reducing or even eliminating the need for catheter use, with faster recovery times.
The most important step is to talk openly with your doctor about your symptoms and concerns. Your experience with BPH is unique, and your treatment plan should be custom to you.
At ProMed DME, we support men on their urinary health journeys. We provide reliable delivery of high-quality catheter supplies, drainage bags, and other urology products, taking one worry off your plate. We offer free shipping across the U.S., a dedicated nurse on staff, and we work with most insurance plans to minimize your costs. Though based in Stuart, Florida, we serve the entire country with care and respect.
Find the right urology supplies for your needs and let us be part of your support system. Your path to better urinary health starts with understanding your options.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



