Sense and Sensibility: Navigating the World of Diabetes Sensors

Why Diabetes Sensors Are Revolutionizing Blood Sugar Management
A diabetes sensor is a small device that continuously tracks your blood sugar levels throughout the day and night. These sensors, also called Continuous Glucose Monitors (CGMs), measure glucose in the fluid under your skin and send real-time data to your smartphone or receiver.
Top Diabetes Sensor Options:
- Dexcom G7 - Most accurate system (8.2% MARD), 10-day wear, smartphone integration
- FreeStyle Libre 3 - World's smallest sensor, 15-day wear, real-time readings every minute
- Eversense 365 - Only year-long sensor, implantable, removable transmitter
- Stelo - Over-the-counter option, no prescription needed, for adults not on insulin
Gone are the days when managing diabetes meant constantly pricking your finger. Today's diabetes sensors provide 24/7 glucose monitoring with minimal finger sticks required. As one user shared, "I love that you get readings every minute; it makes me feel like I have full control of my levels."
These devices work by measuring glucose in your interstitial fluid - the liquid surrounding your cells. The glucose level here closely follows your blood sugar, typically within 5 minutes of changes. Most sensors are waterproof, discreet, and designed for active lifestyles.
The benefits are clear: improved A1C levels, more time in healthy glucose ranges, and peace of mind through customizable alerts. Studies show that people using CGMs have fewer dangerous low blood sugar episodes and better overall diabetes control.
Whether you're looking for a prescription CGM for insulin management or an over-the-counter sensor for lifestyle insights, the right diabetes sensor can transform how you understand and manage your health.
The Benefits of Continuous Monitoring
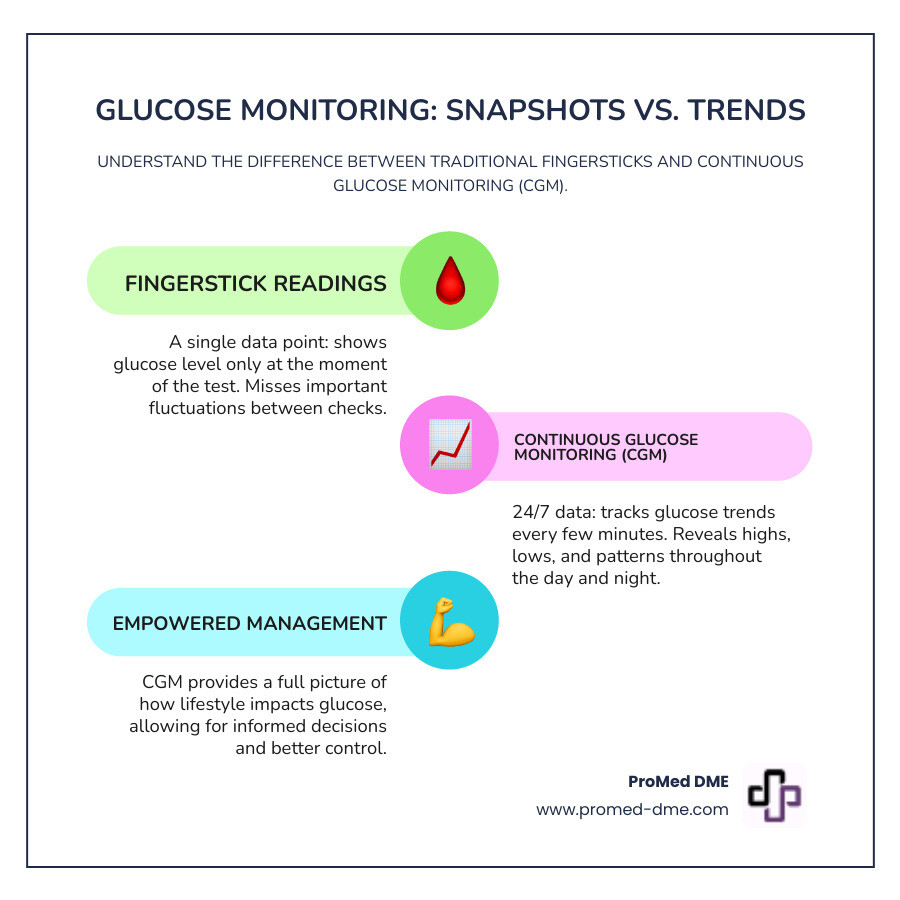
Picture this: you're managing your diabetes with just four fingersticks a day. That's like trying to watch a movie by looking at four random screenshots. You miss all the action, the plot twists, and the important moments in between.
That's exactly why diabetes sensor technology is changing everything. Instead of those isolated snapshots, you get the full story of what's happening with your blood sugar 24/7.
Improved diabetes management becomes so much easier when you can see the complete picture. Your glucose naturally rises and falls throughout the day based on what you eat, how you move, your stress levels, and even how well you sleep. With continuous monitoring, you start noticing patterns you never knew existed. Maybe your blood sugar spikes every Tuesday afternoon (hello, work stress!), or perhaps that "healthy" granola bar sends your levels on a roller coaster ride.
This detailed insight leads to something really exciting: lower A1C levels and more time in your target range. Studies consistently show that people using continuous glucose monitors achieve better long-term control. Your A1C - that important number that shows your average blood sugar over three months - often improves significantly. More importantly, you spend more time in that sweet spot where your glucose levels should be.
But here's what many people don't expect: the incredible peace of mind that comes with continuous monitoring. No more wondering "what's my blood sugar right now?" or worrying about dangerous lows while you sleep. The customizable alerts act like a helpful friend, gently letting you know when your levels are heading out of range - before you feel sick or shaky.
One of the most valuable features is data sharing with caregivers. Your spouse can get alerts if your blood sugar drops during the night. Your adult children can check on you without calling every few hours. Your healthcare team gets real data instead of trying to piece together what happened between appointments.
Perhaps the most empowering benefit is understanding how your lifestyle impacts your glucose. You'll find which foods work best for your body, how different types of exercise affect your levels, and even how emotions influence your blood sugar. It's like having a personal detective helping you solve the mystery of your metabolism.
This knowledge transforms diabetes management from guesswork into informed decision-making. You're no longer reactive - you become proactive about your health.
At ProMed DME, we understand how life-changing this technology can be. We're here to help you steer insurance coverage, find the right system for your lifestyle, and provide ongoing support. More info about our diabetes care services is available to help you take this important step forward in managing your health.
Choosing Your Ideal Diabetes Sensor

Finding the right diabetes sensor depends on your unique lifestyle, health goals, and preferences. Consider your daily routine: are you highly active, or do you prefer minimal device maintenance? Key factors include sensor type (on-skin vs. implanted), wear time (ranging from 10 days to a full year), accuracy, and overall lifestyle fit. Let's explore the three main categories to help you find your match.
Short-Wear Transdermal Sensors (10-15 Days)
These are the most common type of diabetes sensor, offering a great balance of convenience and performance. They feature a self-applied, disposable all-in-one design; you simply apply a new sensor at home every 10-15 days. These sensors send real-time data to your smartphone, often with fast warm-up times (some in 30 minutes). They are discreet and waterproof, making them ideal for active lifestyles as you can shower, swim, or exercise without interruption. The newest models are tiny and highly accurate, rivaling traditional fingerstick tests.
Long-Wear Implantable Sensors (6-12 Months)
For those wanting a "set it and forget it" approach, implantable sensors are the longest lasting sensor option. A small sensor is inserted under the skin in a quick in-office procedure. A removable smart transmitter sits on the skin above it, which can be taken off as needed. Users benefit from exceptional accuracy, minimal false compression lows (false alarms from sleeping on the sensor), and reduced sensor changes. While it requires an initial procedure, it provides 6-12 months of convenient monitoring.
Over-the-Counter (OTC) Biosensors
Excitingly, glucose monitoring is now available without a prescription. OTC biosensors are designed for adults not on insulin who want to understand how lifestyle choices affect their glucose levels. With a focus on lifestyle and diet insights, they help you understand metabolic health by revealing how your body responds to food, exercise, and stress. A 15-day wear period provides ample data to see patterns. These sensors are a tool for health optimization, not medical treatment. Always consult your healthcare provider before making significant health decisions based on this data.
Choosing the right diabetes sensor can feel overwhelming. The ProMed DME team is here to help you steer insurance, compare systems, and find the solution that fits your life.
How to Get Started with a CGM

Getting your first diabetes sensor might feel overwhelming, but it's actually much simpler than most people think. The good news? You don't have to steer this journey alone. We've helped thousands of people get started with CGM systems, and we're here to walk you through every step of the process.
Your journey begins with a conversation with your healthcare provider. This isn't just a formality – it's your opportunity to discuss which type of diabetes sensor makes the most sense for your lifestyle and medical needs. Your doctor will assess whether a CGM is right for you, especially if you're on insulin therapy or have experienced problematic low blood sugar episodes. Even if you're considering an over-the-counter option like Stelo, talking with your healthcare provider first gives you valuable context about how glucose monitoring fits into your overall health picture.
Once your doctor determines that a CGM would benefit you, they'll write a prescription. This is where many people worry about costs, but here's some encouraging news: Medicare Part B covers systems like the Dexcom G7 for eligible individuals, particularly those on insulin or with a history of dangerous low blood sugar. Many commercial insurance plans also provide excellent coverage – some users of the Eversense 365 system pay as little as $199 for an entire year of monitoring.
This is exactly where ProMed DME makes your life easier. Insurance verification can be confusing and time-consuming, but our team handles all the paperwork for you. We work with most insurance plans and understand exactly how to maximize your benefits while minimizing your out-of-pocket costs. No more calling insurance companies or trying to decode coverage policies – we've got you covered.
What really sets us apart is our commitment to making this process seamless for you. We offer free shipping directly to your door because we believe getting your essential medical supplies shouldn't add stress to your life. But perhaps most importantly, we have a dedicated nurse on staff who's available to answer your questions about using your new diabetes sensor. Whether you're wondering about sensor placement, troubleshooting an app issue, or just need reassurance that you're doing everything correctly, our nurse is there to support you.
Here's how simple it is to get your CGM through ProMed DME:
- Talk to your doctor about getting a CGM prescription
- Contact us at ProMed DME – we'll take it from there
- We handle your insurance verification and all the paperwork
- Your supplies ship free directly to your home
- Our nurse is available to answer any questions about your new device
For over-the-counter biosensors, the process is even more straightforward since no prescription is required. You can purchase these directly, though we still recommend that initial conversation with your healthcare provider to ensure an OTC option aligns with your health goals.
The truth is, starting with a diabetes sensor doesn't have to be complicated. With the right support team – like ours at ProMed DME – you can go from prescription to confidently using your new CGM in just a few days. We're here to make sure you feel supported every step of the way.
Considerations and Best Practices for Your Diabetes Sensor

To get the most from your diabetes sensor, it's important to understand some practical realities of the technology.
Cost and insurance coverage are common concerns. Without insurance, CGMs can cost $100-$300 monthly. Fortunately, most plans, including Medicare Part B for eligible individuals, now offer coverage. At ProMed DME, we are experts at navigating insurance to minimize your out-of-pocket costs, handling the paperwork and exploring assistance programs for you.
Understanding accuracy and MARD scores sets realistic expectations. MARD (Mean Absolute Relative Difference) measures how close CGM readings are to fingerstick results—a lower score is better. A MARD score in the 8-9% range, like the Dexcom G7's 8.2%, is considered excellent and indicates a highly accurate system.
A diabetes sensor measures glucose in the fluid around your cells, not directly in your blood. This causes a brief interstitial fluid lag of about five minutes. This delay is normal and most noticeable when your blood sugar is changing rapidly, such as after meals or during exercise.
Alarm fatigue can be a challenge. Frequent alerts may cause you to become less responsive. Work with your healthcare provider to set thresholds that are helpful but not disruptive.
Some users experience skin adhesive irritation. Redness or itching can develop, especially with sensitive skin. Different systems use different adhesives; for example, the Eversense system uses a gentle, silicone-based adhesive changed daily. If irritation persists, talk to your provider about trying different sites, barrier creams, or other CGM options.
Safety warnings are critical. Always follow device instructions. If your glucose alerts and readings don't match how you feel, trust your body and confirm with a fingerstick check before making treatment decisions. Never ignore your symptoms.
Don't adjust medication based only on sensor readings without consulting your provider. Certain medications like acetaminophen, hydroxyurea, or high doses of Vitamin C can interfere with CGM accuracy, so check with your doctor when starting new medications.
For those using over-the-counter CGMs, remember these are for lifestyle insights, not medical decision-making. They are powerful tools but don't replace professional medical guidance, especially if you're on insulin.
The world of CGM technology continues to evolve, with researchers exploring applications beyond diabetes management. If you're curious about the broader potential of this technology, this scientific research on CGM use by people without diabetes offers fascinating insights into how these devices might help optimize health for everyone.
Every person's experience with a diabetes sensor is unique. Stay informed, communicate with your healthcare team, and take time to learn how your system works best for your lifestyle.
Frequently Asked Questions about Diabetes Sensors
We hear many of the same questions from customers about continuous glucose monitoring. Let's explore the most common concerns to help you feel confident about making the switch to a diabetes sensor.
How accurate are CGM systems?
Modern diabetes sensor systems are remarkably accurate. Accuracy is measured using a MARD score explanation. MARD (Mean Absolute Relative Difference) shows how close CGM readings are to blood glucose levels—a lower score is better.
An 8-9% range is excellent for any CGM system. For example, the Dexcom G7 has a MARD of 8.2%, making it one of the most precise systems available.
While fingersticks provide a single snapshot, a diabetes sensor offers continuous data to reveal trends. There is a small physiological delay, as CGMs measure glucose in the fluid around your cells, not directly in the blood.
This is why the importance of confirming with a blood glucose meter when symptoms don't match readings is critical. If you feel shaky but your CGM shows normal levels, trust your body and perform a fingerstick check, especially when glucose levels are changing rapidly.
Do I still need to do fingerstick checks with a CGM?
While you'll need far fewer fingersticks, it's smart to keep backup supplies handy.
Most modern CGMs are factory-calibrated, eliminating the need for the routine fingerstick checks required by older systems. However, calibration requirements for some systems still exist. Some sensors may require occasional checks to maintain accuracy, so always check your specific device's requirements.
The most important time for confirming questionable readings is when your symptoms don't match the device. If your CGM reads 120 mg/dL but you feel low, use your backup meter to verify. Backup supplies are also a safety net for sensor malfunctions, ensuring you always have a way to monitor your glucose.
Understanding when to trust your body over the device is crucial. Always take physical symptoms seriously and use a fingerstick to confirm when in doubt.
Can I get a CGM without a doctor's prescription?
Yes, certain diabetes sensor systems are now available without a prescription, but it's important to understand who they are for.
Over-the-counter (OTC) options like the Stelo Glucose Biosensor System can be purchased directly, making glucose insights more accessible. The indications for OTC use are specific: they are for adults 18 and older who are not on insulin. They are valuable for understanding how lifestyle choices impact glucose levels.
However, consult a healthcare professional for medical decisions. OTC sensors are wellness tools for insight, not for making medical treatment decisions without professional guidance.
Crucially, these systems are not for insulin users. Managing diabetes with insulin requires the precision and oversight of prescription-grade CGM systems for safe treatment adjustments. For insulin users, prescription systems are the gold standard, offering clinical-grade accuracy and insurance coverage. Our team at ProMed DME specializes in helping customers steer insurance for these devices to reduce out-of-pocket costs.
Take Control of Your Health Today
The journey through continuous glucose monitoring might feel overwhelming at first, but you've just finded something truly remarkable. Diabetes sensor technology isn't just changing how we manage diabetes – it's completely revolutionizing what it means to live well with this condition.
Think about the empowerment through technology that's now at your fingertips. Instead of wondering what your blood sugar did overnight or how that slice of pizza affected you three hours later, you'll have real answers. Every meal choice, every walk around the block, even how a stressful day at work impacts your glucose – it all becomes clear. This isn't just data; it's the foundation for making informed decisions that actually work for your unique body and lifestyle.
What we hear most from our customers is how dramatically their quality of life improves. One person told us they finally felt like they could travel without anxiety. Another said they stopped waking up in the middle of the night worried about their levels. These aren't small changes – they're life-changing shifts that happen when you have reliable, continuous information about your health.
Your diabetes sensor becomes more than just a device you wear. It transforms into your personal health partner, working 24/7 to keep you informed and safe. Whether you choose a short-wear system for its convenience, a long-wear implantable for minimal maintenance, or an over-the-counter option to understand your metabolic health better, you're choosing to take an active role in your wellbeing.
We understand that starting this journey can feel daunting, especially when you're dealing with insurance questions, device options, and learning new technology. That's exactly why we're here. Our team handles the complicated insurance paperwork, our dedicated nurse answers your questions (no matter how small they seem), and we ship everything directly to your door at no extra cost.
Every person deserves to feel confident and in control of their health. Whether you're managing Type 1 diabetes, Type 2 diabetes, or simply want to optimize your metabolic health, continuous glucose monitoring can be the game-changer you've been looking for.
Ready to see what a difference continuous monitoring can make in your daily life? We're here to help you every step of the way, from choosing the right system to getting it covered by your insurance.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



