Sensor-Augmented Pumps: Taking Insulin Therapy to the Next Level

Why Sensor-Augmented Pumps Are Changing Diabetes Care
Sensor augmented insulin pump therapy combines an insulin pump with continuous glucose monitoring to create a smart system that helps manage diabetes more effectively than traditional methods.
Quick Overview:
- What it is: An insulin pump connected to a continuous glucose monitor (CGM)
- How it works: The CGM sends real-time glucose data to the pump for better insulin delivery decisions
- Key benefits: Better blood sugar control, fewer dangerous lows, improved quality of life
- Who it helps: People with Type 1 diabetes and insulin-requiring Type 2 diabetes
- Results: Studies show HbA1c drops from 8.3% to 7.5% compared to 8.3% to 8.1% with injections
Managing diabetes with traditional insulin injections can be a full-time job, requiring constant finger sticks, meal planning, and guesswork. Sensor-augmented pumps are a major step forward, providing real-time glucose readings every few minutes instead of leaving you to guess between tests.
The system acts as a co-pilot for your diabetes management. The continuous glucose monitor constantly watches your blood sugar trends, and the insulin pump delivers precise insulin doses based on that real-time information.
Research shows impressive results. In a major study of 485 patients, those using sensor-augmented pump therapy saw their average HbA1c levels drop to 7.5%, while those on traditional injections only improved to 8.1%. Furthermore, 27% of pump users reached the target HbA1c of 7% or less, compared to just 10% of injection users.

Glossary for sensor augmented insulin pump therapy:
- continuous glucose monitoring system
- aace guidelines for insulin pump therapy
- candidates for insulin pump therapy
How Sensor-Augmented Pumps (SAPs) Work
Sensor augmented insulin pump therapy combines two key technologies that work as a team to manage diabetes more effectively than either could alone.

The insulin pump is a small device that delivers insulin continuously (a basal rate) through a tiny tube inserted just under your skin. When you eat or need to correct high blood sugar, you instruct it to deliver a bolus dose. This method, called continuous subcutaneous insulin infusion (CSII), mimics the body's natural insulin release more closely than injections.
The continuous glucose monitor (CGM) acts as a watchful guardian. A tiny glucose sensor inserted into the interstitial fluid under your skin measures glucose levels every few minutes. It then sends that information wirelessly through a transmitter to your pump or phone.
The power of this partnership is the real-time data flowing between the devices. Your pump isn't delivering insulin blindly; it's getting constant updates. For healthcare providers wanting to learn more, this overview of insulin pumps and glucose sensors provides excellent technical details.
What Makes SAPs Different from Traditional Pumps?
The key difference is manual input versus data integration. Instead of relying on single-point-in-time fingersticks and guesswork, SAPs use a constant stream of data from the CGM. This allows for proactive adjustments rather than reactive ones. For example, when your glucose starts dropping, the pump can see the trend and automatically reduce or stop insulin delivery before you experience a low.
Trend arrows on your pump screen show whether your glucose is rising, falling, or holding steady, while predictive alerts warn you about potential highs or lows before they happen. Most current systems are open-loop systems, meaning you are still in control of major decisions about meals and corrections, but you're working with much better information.
The Role of the Continuous Glucose Monitor (CGM)
Your CGM does the hard work of tracking your blood sugar 24/7. Sensor insertion is simple, using an automatic applicator to place a tiny, flexible sensor that typically lasts for about a week.
Most CGMs still need calibration with a fingerstick test once or twice a day to ensure accuracy. It's best to calibrate when your blood sugar is stable. This process dramatically reduces the need for frequent daily fingersticks, saving your fingertips and providing a more complete picture of your glucose levels.
Understanding glucose trends becomes intuitive. Trend arrows help you stay ahead of problems, and tracking your time in range—the percentage of time your glucose stays between 70-180 mg/dL—becomes a motivating and useful goal. Research shows that people who use their sensor more than 80% of the time see the biggest improvements in their blood sugar control.
The Benefits of Sensor Augmented Insulin Pump Therapy
Sensor augmented insulin pump therapy provides the tools to move beyond the constant balancing act of diabetes management, giving you the information needed to stay safely in control.
Users experience improved HbA1c levels, reduced hyperglycemia (high blood sugar), and most importantly, hypoglycemia prevention. These clinical benefits lead to significant quality of life improvements, including less worry, better sleep, and more stable moods. This increased confidence is reflected in higher treatment satisfaction scores in research studies. Scientific research on hypoglycemia prevention continues to demonstrate how transformative these systems can be.
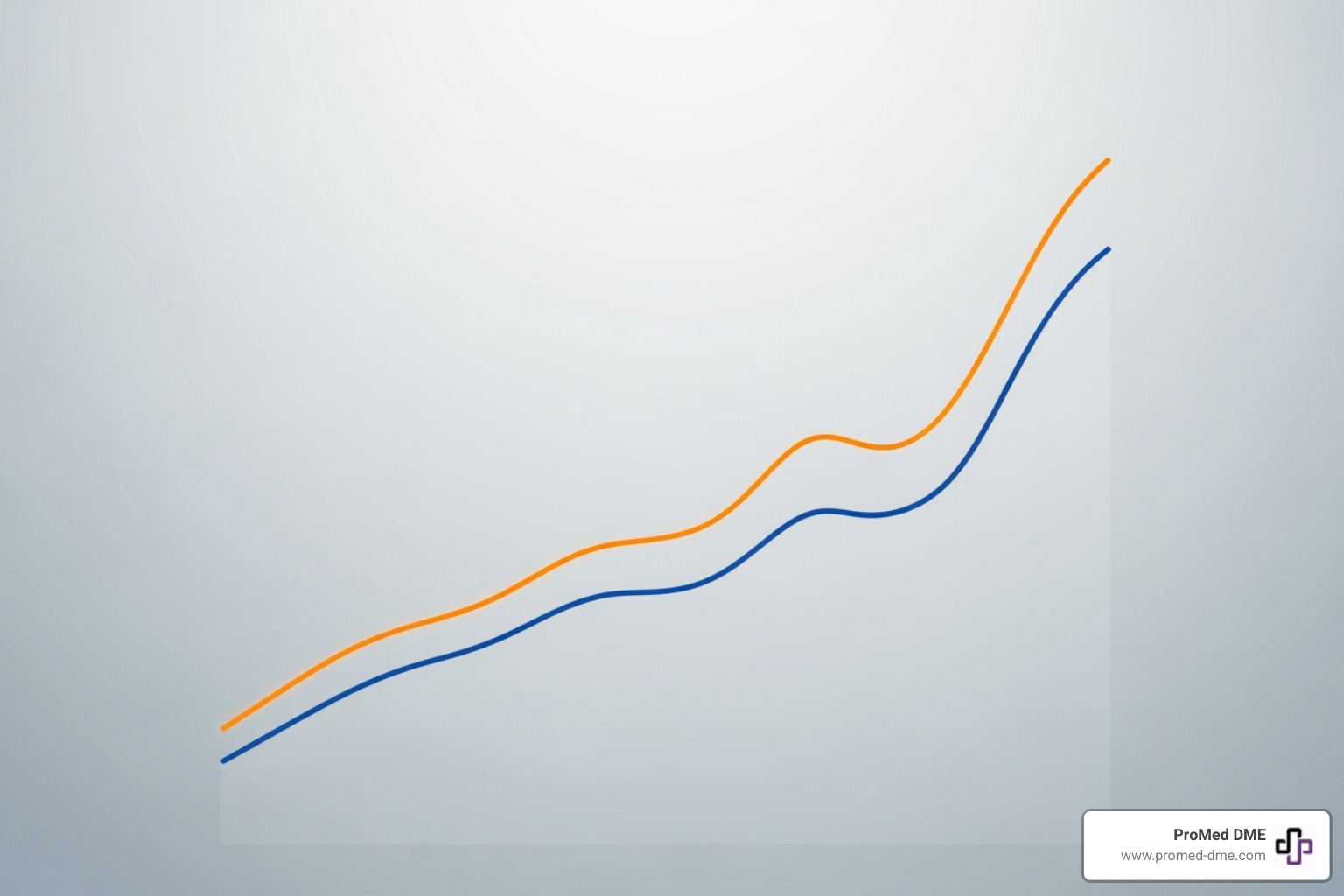
Better Glycemic Control Compared to MDI
Research clearly shows superior glycemic control with SAP therapy compared to multiple daily injections (MDI). In a year-long study, SAP users saw their average HbA1c drop from 8.3% to 7.5%, while MDI users only improved from 8.3% to 8.1%. This means more than one in four people using the sensor-augmented system reached the recommended HbA1c target of 7% or less, while only one in ten on injections achieved that goal.
Beyond better averages, users experience reduced glucose variability, meaning fewer blood sugar roller coasters. The table below highlights the key differences.
| Outcome | Sensor Augmented Insulin Pump Therapy | Multiple Daily Injections (MDI) |
|---|---|---|
| Mean HbA1c at 1 Year | 7.5% | 8.1% |
| % Reaching HbA1c ≤ 7% | 27% | 10% |
| Severe Hypoglycemia Rate (per 100 PY) | 13.31 | 13.48 |
| Reduction in Hyperglycemia | Significant | Less significant |
Importantly, this better control did not increase the rate of severe hypoglycemic events, which remained nearly identical between the groups, proving you can achieve better control and safety simultaneously.
Preventing and Managing Hypoglycemia
For many, the fear of low blood sugar is a constant challenge. This is where sensor augmented insulin pump therapy truly shines. The low glucose suspend feature acts as a safety net, automatically stopping insulin delivery when the CGM detects falling glucose levels.
More advanced systems use predictive low glucose suspend, which looks at your glucose trends to anticipate and prevent an impending low before it happens. This automated insulin suspension is a game-changer for people with hypoglycemia unawareness (not feeling the warning signs of a low).
The psychological benefits are immense. The constant fear of hypoglycemia fades, especially improving nighttime safety, as the system works while you sleep. Users report better sleep and more confidence to travel, exercise, and live life with less worry.
Using and Understanding Your SAP System
Getting started with an SAP system involves working with your healthcare team to personalize settings that match your body's needs. Once you learn the basics, the system becomes an intuitive part of your daily routine.

Your therapy is built on basal and bolus settings. Basal rates provide steady background insulin, while bolus doses cover meals and correct high blood sugar. Your pump's bolus calculator uses your personalized insulin-to-carb ratio and correction factor to suggest precise doses, taking the complex math out of your hands.
Key Features of Sensor Augmented Insulin Pump Therapy
Modern SAP systems are packed with features designed to simplify diabetes management:
- Temporary Basal Rates: Give you flexibility to reduce insulin for exercise or increase it during illness.
- Customizable Alerts: You can set high and low glucose alarms that fit your comfort level and lifestyle.
- Active Insulin Time: Tracks how long insulin is working in your body to prevent "stacking" doses and causing a low.
- Data Sharing: Your pump and CGM data can be shared with your healthcare provider, making appointments more productive.
- Bolus Delivery Options: Features like square wave or dual wave boluses help manage insulin delivery for different types of meals, such as high-fat foods.
Potential Risks and How to Mitigate Them
While SAP therapy is safe and effective, it's important to be aware of potential issues and how to prevent them.
- Infusion Site Issues: Rotate your infusion site every 2-3 days to prevent irritation, infection, or kinking.
- Skin Irritation from Sensors: If you have sensitive skin, try different sensor locations or use barrier wipes for protection.
- Sensor Accuracy Problems: Modern CGMs are very accurate, but if a reading seems off, especially during rapid glucose changes, confirm with a fingerstick.
- Ketoacidosis Risk from Pump Failure: Since you're not taking long-acting insulin, a pump malfunction can lead to a rapid lack of insulin. Always have backup supplies—including insulin pens and extra infusion sets—readily available.
- Over-reliance on Technology: The system is a co-pilot, not an autopilot. Your active engagement is essential for success.
- Nuisance Alarms: Work with your provider to find the right alert settings to keep you safe without causing frustration.
The Evolution Toward an Artificial Pancreas
Sensor augmented insulin pump therapy is a crucial stepping stone toward the artificial pancreas—a fully automated, closed-loop system that was once science fiction.
Today's hybrid closed-loop systems are a reality. They feature automated basal insulin delivery, where a smart algorithm constantly learns your patterns and adjusts background insulin 24/7. While you still need to tell the system about meals, it handles the constant micro-adjustments that keep your glucose more stable.
This technology is here now, changing how people manage their diabetes every day. The future of diabetes care is unfolding before our eyes. For those interested in a deeper dive, Current diabetes technology: Striving for the artificial pancreas offers excellent insights.
Latest Advancements in SAP Technology
The world of SAP technology moves quickly. Key innovations include:
- Smarter Algorithms: These programs learn your individual patterns and can even deliver automated correction insulin if you forget to bolus.
- Improved Sensor Accuracy: Newer sensors are more reliable and respond faster to glucose changes.
- Extended Sensor Wear Time: Some models can be worn for two weeks or longer, increasing convenience.
- Smartphone Integration: Many systems allow you to view data and even control your pump directly from your phone.
- Tubeless Pump Options: These patch pumps offer greater freedom of movement and are becoming more integrated with advanced algorithms.
- Interoperability: The goal is a future where you can mix and match your favorite CGM and insulin pump, regardless of the manufacturer.
Is Sensor Augmented Insulin Pump Therapy Right for You?
SAP therapy can be life-changing, but it requires commitment. Consider if it's a good fit for you:
- Candidate Criteria: You have Type 1 or insulin-requiring Type 2 diabetes and are struggling to meet your goals with other methods.
- Technology Comfort: You don't need to be an expert, but you should be willing to learn and interact with a device.
- Commitment to Engagement: The system works best when you are actively involved. You'll still count carbs and respond to alerts. Consistent sensor use is key to success.
- Lifestyle Considerations: It's especially helpful for those with active lifestyles, irregular schedules, or who travel frequently.
- Key Motivators: A strong desire for better control or a history of severe lows or hypoglycemia unawareness makes you an excellent candidate.
Discuss these points with your healthcare provider to make an informed decision. At ProMed DME, we work with providers to help patients access the right technology for their needs.
Getting Started with SAP Therapy
Taking the leap into sensor augmented insulin pump therapy is a big step. Understanding the financial and practical aspects can make the process much smoother.
The initial cost for an insulin pump is around $6,000, with ongoing annual supply costs for infusion sets, reservoirs, and CGM sensors ranging from $3,000 to $6,000. While this is a significant investment, it should be weighed against the long-term health benefits, improved quality of life, and reduced risk of costly complications.
Insurance Coverage is a key consideration. The good news is that most insurance plans, including Medicare and Medicaid, typically cover insulin pump therapy and supplies. However, coverage details vary, and the process can be complex.
This is where a Durable Medical Equipment (DME) provider like ProMed DME can help. We work directly with most insurance plans and handle the prior authorization paperwork to minimize your out-of-pocket expenses. Our dedicated nurse on staff can guide you through the process, and with free shipping delivered to your door, getting your supplies is simple and convenient.
Important Questions for Your Healthcare Provider
Starting SAP therapy is a partnership with your healthcare team. Being prepared with questions will build your confidence. Here are some key topics to discuss:
- Training & Setup: What does the training involve? How will my initial pump settings (basal/bolus rates, correction factors, carb ratios) be determined?
- Daily Management: What is our plan for sick days? Who should I contact for technical support—the clinic or the manufacturer?
- Practical Use: How should I adjust insulin for exercise? When should I take my bolus for meals?
- Safety & Backup: What should I do if my blood sugar drops despite the pump's safety features? What backup supplies (insulin pens, extra sets) should I always have on hand?
- Follow-up Care: How often will we review my pump and CGM data together? What is the process for getting ongoing supplies?
Conclusion
Sensor augmented insulin pump therapy is one of the most significant breakthroughs in modern diabetes care. It transforms daily management from a constant guessing game into a safer, more predictable experience.
The results are clear. Studies show that people switching to SAP therapy see their HbA1c levels drop significantly (from 8.3% to 7.5%), and nearly three times as many users reach their target HbA1c of 7% or less compared to those on injections.
Beyond the statistics, this technology empowers you to live your life more fully. The system's safety features and real-time data provide confidence and peace of mind, reducing the fear of hypoglycemia and allowing for greater flexibility. It is your gateway to the future of diabetes care, which continues to evolve toward a fully automated artificial pancreas.
At ProMed DME, we understand that navigating new technology and insurance coverage can be overwhelming. Our team is here to make the process as smooth as possible. With a dedicated nurse on staff, free shipping, and experience working with most insurance plans, we help you access these life-changing supplies with minimal out-of-pocket costs.
We believe everyone deserves access to the best diabetes technology available. With the right tools and a supportive team, you can take charge of your diabetes and live the life you want.
For more information about diabetes management supplies, please visit promeddme.com/diabetes-care/.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.


