A Comprehensive Guide to DME BCBS Coverage

Why Understanding Durable Medical Equipment Blue Cross Blue Shield Coverage Matters
Navigating durable medical equipment blue cross blue shield coverage can be overwhelming. When you're managing a health condition, the last thing you need is confusion about insurance. This guide simplifies the process.
Quick Answer: What You Need to Know
To get DME covered by Blue Cross Blue Shield, you must:
- Get a prescription from your doctor.
- Prove medical necessity - the equipment must treat your condition.
- Use in-network suppliers to minimize costs.
- Know your plan type - Standard vs. Basic options have different costs.
- Verify coverage before ordering.
Common covered items include wheelchairs, hospital beds, oxygen equipment, and CPAP machines. Items not covered are for comfort, home modifications, or general exercise.
Because BCBS is a network of independent companies, policies can vary by state. This guide will walk you through the criteria, coverage details, and approval process to help you save money and avoid denials.
Simple guide to durable medical equipment blue cross blue shield terms:
Understanding DME and Blue Cross Blue Shield Coverage Criteria
Durable medical equipment (DME) is reusable medical gear that helps you manage a health condition at home. To qualify for durable medical equipment blue cross blue shield coverage, the item must meet several key criteria, which are often aligned with Medicare guidelines.
Key Criteria for DME Coverage
BCBS will only cover equipment that is:
- Prescribed by your doctor: A physician, PA, or NP who is treating you must write a prescription.
- Medically Necessary: This is the most critical factor. The equipment must be essential for treating your illness, improving function, or preventing your condition from worsening. It cannot be for mere comfort or convenience. For example, a pressure-reducing mattress to prevent bed sores is therapeutic, while a standard mattress is for comfort.
- For Medical Use: The item is not something a healthy person would typically use (e.g., a walker vs. an exercise bike).
- Reusable: It's designed for repeated use, distinguishing it from disposable supplies like bandages.
- For Home Use: The equipment must be appropriate for a home setting.
For more details, you can review this guide to medical necessity for DME from a BCBS affiliate.
How Medical Necessity is Determined
To prove medical necessity, your doctor's documentation must tell a clear story. BCBS reviews your physician's treatment plan, the predicted therapeutic outcomes, your current clinical diagnosis, and how your condition impacts your functional ability to perform daily activities. Thorough documentation is the key to a smooth approval process.
What's Covered? Navigating Your Durable Medical Equipment Blue Cross Blue Shield Benefits
Understanding what your durable medical equipment blue cross blue shield plan covers can save you from unexpected bills. While plans vary, most follow similar guidelines.

Typically Covered vs. Not Covered
Most BCBS plans cover a wide range of medically necessary equipment.
Commonly Covered:
- Mobility aids (wheelchairs, scooters, walkers, crutches)
- Hospital beds
- Respiratory equipment (oxygen, CPAP/BiPAP machines, nebulizers)
- Diabetes supplies (insulin pumps and infusion sets)
- Speech-generating devices
- Ostomy supplies
- Pressure mattresses, lymphedema pumps, and TENS units
Typically Not Covered:
- Comfort/Convenience Items: Air conditioners, humidifiers, standard mattresses.
- Home Modifications: Ramps, stair-lifts, grab bars.
- Exercise Equipment: Treadmills, stationary bikes.
- General Supplies: Over-the-counter items not used with covered DME.
Special Considerations and Prior Approval
Expensive or complex items often require prior approval before you order them. This is common for:
- Power wheelchairs: Require strict proof that you cannot use a manual chair and can operate it safely.
- Insulin pumps: Covered for patients who meet specific clinical criteria.
- Speech-generating devices: Often have annual benefit limits (e.g., $625 to $1,250 for FEP plans).
Getting approval first ensures BCBS agrees the item is medically necessary, preventing a costly denial.
Coverage Differences: Standard vs. Basic Plans
Your out-of-pocket cost depends heavily on your plan type and whether you use an in-network provider.
- Standard Plans: Offer more flexibility but have higher premiums. Using a Preferred provider results in the lowest cost-sharing (e.g., 15% coinsurance).
- Basic Plans: Have lower premiums but are much stricter. Going to a non-Preferred provider could mean you are responsible for all charges.
The table below illustrates the dramatic cost differences. This is why we at ProMed DME always help customers verify their coverage to minimize expenses.
| Plan Option | DME Provider Type | Member's Out-of-Pocket Cost (after deductible for Standard) |
|---|---|---|
| Standard | Preferred | 15% of Plan allowance |
| Standard | Participating | 35% of Plan allowance |
| Standard | Non-participating | 35% of Plan allowance + difference between allowance & billed amount |
| Basic | Preferred | 30% of Plan allowance |
| Basic | Participating | All charges |
| Basic | Non-participating | All charges |
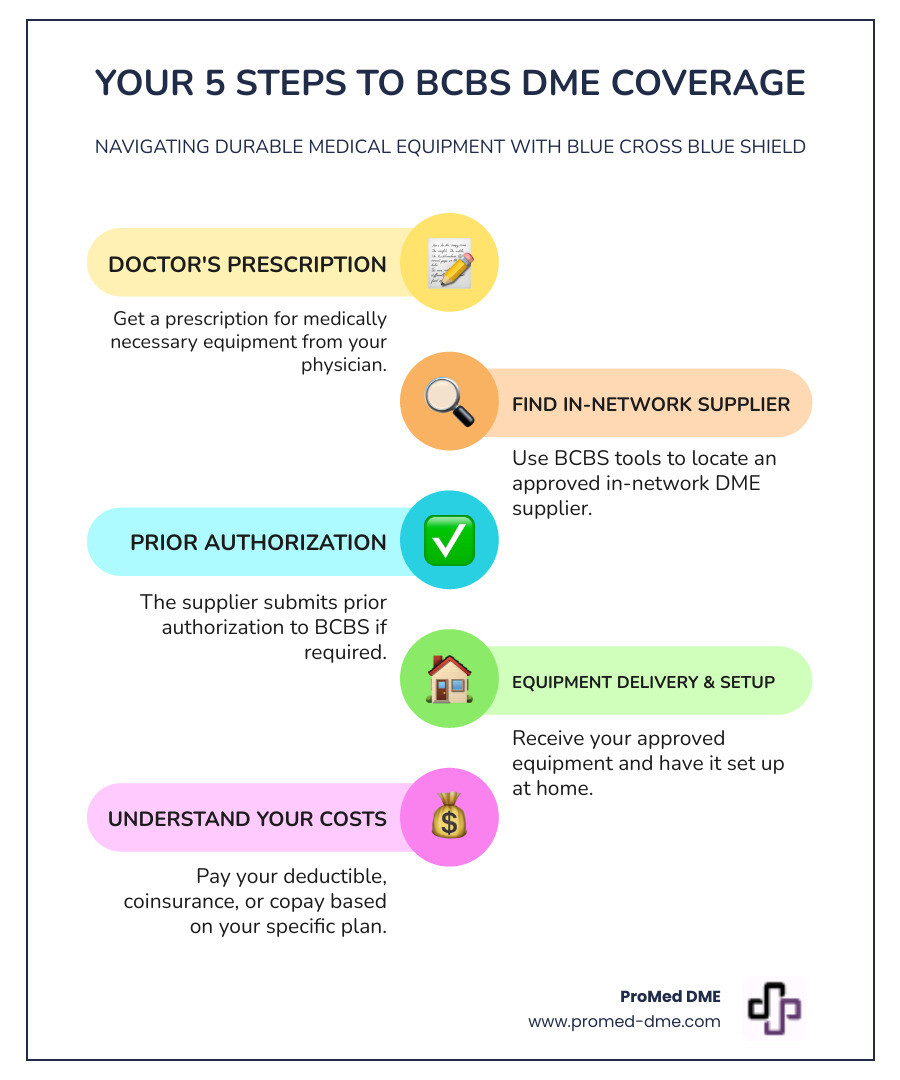
The Process: How to Get Your DME Covered by BCBS
Getting your durable medical equipment blue cross blue shield covered involves a few key steps. Understanding this process makes it much easier to steer.
Step 1: The Doctor's Prescription
Everything begins with a prescription from your attending physician. This isn't just a note; it's a detailed order that must include your diagnosis, the specific equipment needed, the medical reason for it, and the expected duration of use. This document is the foundation for proving medical necessity to BCBS.
Step 2: Finding an In-Network DME Supplier
Your next step is crucial for controlling costs: find the right supplier. BCBS plans use provider networks:
- Preferred providers offer the lowest out-of-pocket costs.
- Participating providers are also in-network but may have higher cost-sharing.
- Non-participating providers have no contract with BCBS, and using them can lead to you paying the entire bill, especially on a Basic plan.
Always verify a supplier is in-network before ordering. Most BCBS plans have online tools to help, like the BCBS Find Care tool. At ProMed DME, we work with most insurance plans to help you maximize your benefits.
Step 3: Prior Authorization and Required Documentation
For expensive or specialized items like power wheelchairs or specialty beds, BCBS requires prior authorization. This means your DME supplier and doctor must submit a request and get approval before you receive the equipment.
This process involves submitting your prescription, medical records, and a Certificate of Medical Necessity (CMN). The CMN is a standard form that summarizes the medical justification for the equipment. An experienced DME supplier can help ensure this paperwork is complete and accurate, which is vital for preventing delays or denials.
Managing Costs and Equipment
Knowing what you'll pay for durable medical equipment blue cross blue shield is as important as knowing what's covered. Let's break down the costs and equipment management.

Understanding Your Out-of-Pocket Costs for durable medical equipment blue cross blue shield
Your final bill depends on your plan's structure:
- Deductible: The amount you pay before your insurance begins to pay.
- Coinsurance: The percentage of the cost you are responsible for after your deductible is met (e.g., 15%, 30%).
- Copayment: A flat fee for certain services or supplies.
- Plan Allowance: The maximum amount your plan will pay for an item. If you use an out-of-network provider who charges more than the allowance, you pay the difference. This is why staying in-network is critical to avoid large, unexpected bills.
At ProMed DME, we verify your benefits upfront so you know what to expect.
Rental vs. Purchase: How BCBS Decides
BCBS decides whether to rent or purchase equipment based on cost-effectiveness and your medical need.
- Rental is common for short-term needs (e.g., a walker after surgery) or for high-maintenance items like oxygen concentrators, where the supplier handles upkeep.
- Purchase is preferred for long-term or permanent needs (e.g., a wheelchair for a chronic condition).
Some items fall under a capped rental policy, where after a set number of rental payments (often 13 months), you own the equipment.
Policy on DME Repair, Maintenance, and Replacement for durable medical equipment blue cross blue shield
- Rental Equipment: The supplier is responsible for all maintenance, repairs, and replacements. This is included in the rental fee.
- Purchased Equipment: You own it, so routine maintenance is your responsibility. However, medically necessary repairs after the warranty may be covered. Replacement is typically covered when the item is past its "expected lifetime" (e.g., 5-7 years for a wheelchair) and no longer meets your medical needs.
Important: Damage from misuse, loss, or theft is generally not covered by BCBS for either rental or purchased items. You would be responsible for these costs.
Special Scenarios and Finding More Information
What about special situations like travel, and where can you find definitive answers about your durable medical equipment blue cross blue shield plan?
DME Coverage While Traveling or Out-of-State
Most BCBS plans cover DME while you are traveling, provided the equipment is also medically necessary at your primary home. You generally cannot get coverage for duplicate equipment just for travel. If you purchase DME while in another state, the local BCBS plan there will typically process the claim. For more details, you can review affiliate policies like this BCN policy on DME while traveling. Before any extended trip, call your plan to confirm coverage.
Defining 'Provider' in the DME Context
In your plan documents, "provider" can have two meanings:
- The DME Supplier: The company that provides the equipment, like ProMed DME.
- The Prescribing Professional: The licensed healthcare professional who orders the equipment. This includes Physicians (MD/DO), Physician Assistants (PAs), and Nurse Practitioners (NPs).
Where to Find Your Specific Plan Details
The most accurate information comes directly from your BCBS plan. Use these resources:
- Your Member Benefit Booklet: The comprehensive guide to your coverage.
- Online Member Portal/App: Check benefits, find providers, and track claims.
- Customer Service Phone Number: Located on your ID card, this is your direct line for answers.
- Summary of Benefits and Coverage (SBC): An easy-to-read overview of your plan's costs.
Always verify your benefits directly with your plan. Our team at ProMed DME is also here to help you steer the insurance process.
Frequently Asked Questions about DME and BCBS Coverage
Here are quick answers to some of the most common questions we hear about durable medical equipment blue cross blue shield coverage.
Do I always need a prescription for DME?
Yes, a prescription from a qualified healthcare provider is non-negotiable. It is the primary document that establishes medical necessity for BCBS, and without it, your claim will be denied.
What happens if my DME claim is denied?
A denial is not the final word. You have the right to appeal.
- Review the denial reason on your Explanation of Benefits (EOB).
- Work with your doctor and DME supplier to gather additional supporting documentation.
- Follow the formal appeals process outlined by your insurance plan.
Many claims are successfully overturned on appeal with the right information.
Are breast pumps covered as DME by Blue Cross Blue Shield?
Yes. Under the Affordable Care Act (ACA), most BCBS plans are required to cover the cost of a breast pump as a preventive benefit for new mothers. However, the type of pump (manual, electric, or hospital-grade rental) and the process for obtaining it vary by plan. Check with your specific BCBS plan to understand your coverage, which suppliers are in-network, and what documentation is needed.
Conclusion
Navigating durable medical equipment blue cross blue shield coverage is manageable when you know the rules. Remember these key takeaways:
- A doctor's prescription is essential to prove medical necessity.
- Always verify your benefits and use in-network suppliers to save money.
- Thorough documentation is crucial for a smooth approval process, especially for items requiring prior authorization.
At ProMed DME, we are your partner in this process. We understand the complexities of insurance and are committed to making it as painless as possible. With free shipping, a dedicated nurse on staff, and expertise in working with most insurance plans, we help minimize your out-of-pocket costs. Your health is too important to let paperwork stand in the way.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



