Managing Elderly Urinary Incontinence: A Comprehensive Guide

As people age, dealing with physical changes and health issues become an intrinsic part of life. Among many age-related health problems, urinary incontinence—a symptom of impaired bladder function—stands as a prevalent and distressing concern in elderly individuals. This medical issue not only imparts discomfort but also carries a significant psychological burden, impacting people's lifestyle and social interactions.
At ProMed DME, we recognize the challenge of managing elderly urinary incontinence. Guided by our expert staff, we extend unmatched assistance in providing the right medical supplies and aiding in seamless prescription procurement, aiming to simplify the journey towards better health. Therefore, we have crafted this comprehensive guide to provide a detailed and empathic understanding of urinary incontinence in the elderly, enlightening on the causes, symptoms, management strategies, and treatment options.
Quick Snapshot
- Urinary incontinence, common in elderly individuals, is a distressing condition resulting from impaired bladder function, structural changes, neural control impairment, or related to medication side effects.
- Depending on the root cause it manifests as stress incontinence, overactive bladder, or mixed incontinence.
- Symptoms may range from slight leakage during activities to a sudden urge for urination that may lead to incontinence before reaching the toilet.
- Early diagnosis and management measures, including medication, behavioral modifications, bladder training, pelvic floor contraction and lifestyle changes, can mitigate the severity and impacts.
- Minimal invasive surgical techniques may be considered for operable patients.

Understanding Urinary Incontinence in the Elderly
As we age, our bodies go through many changes, and the urinary system is no exception. One of the common issues that arises is urinary incontinence — a condition that many seniors grapple with silently. But it doesn't have to be that way. At ProMed DME, we believe in empowering you with the knowledge to manage your health effectively. So let's dive right into understanding urinary incontinence in the elderly: its definition, its types, and its prevalence.
Defining Urinary Incontinence
Urinary incontinence is the involuntary leakage of urine, a symptom of impaired bladder function that is common in the elderly. It's not a disease in itself but a sign of an underlying condition or an effect of certain medications. This involuntary loss of bladder control can vary in intensity from a minor leak when you cough or sneeze to having an urgent need to urinate that's so sudden you don't get to a toilet in time.
Common Types of Urinary Incontinence
Now, it's important to note that not all incontinence is the same. There are several types of urinary incontinence:
- Urgency incontinence, characterized by a sudden need to urinate that's hard to ignore.
- Stress incontinence occurs when physical movement or activity — such as coughing, sneezing, running, or heavy lifting — puts pressure (stress) on your bladder, causing leakage.
- Overflow incontinence, often due to bladder outlet obstruction or an underactive bladder muscle, results in constant minor dribbling of urine.
- Functional incontinence, also known as "Disability-associated" incontinence, is related to difficulty getting to the toilet in time.
- And lastly, some people may experience mixed incontinence, a combination of the above symptoms.
Understanding the type of incontinence you or your loved one is experiencing is the first step in managing the issue effectively.
The Prevalence of Urinary Incontinence in Older Adults
The prevalence of urinary incontinence in the elderly is more common than you might think. In fact, it's estimated that more than 2 million people over the age of 60 in Germany alone are living with urinary incontinence. And the numbers rise even more dramatically for those over 80, with almost 30% affected.
But remember, urinary incontinence is not an inevitable part of aging. Many causes of incontinence are treatable, and even when it's not fully curable, there are many ways to manage the symptoms and improve quality of life. That's where we at ProMed DME come in, offering quality medical supplies and expert advice for managing incontinence and other health concerns. So stay tuned as we delve into the causes, symptoms, and management strategies for urinary incontinence in the elderly in the sections to follow.
Causes of Urinary Incontinence in the Elderly
Understanding the causes of urinary incontinence in the elderly is the first step towards effective management and treatment. The causes can be complex and multifaceted, stemming from age-related changes in the urinary system, medical conditions and medications, as well as lifestyle factors.
Age-Related Changes in the Urinary System
As we age, structural changes in vesical muscle and impaired neural control can lead to urinary incontinence. The capacity to remain continent in old age is influenced by changes in neurogenic control and weakening compensatory mechanisms. Particularly, nerve issues can disrupt the coordination between the brain and the bladder, leading to urinary retention. This lack of coordination can cause the bladder muscle to tighten, squeezing urine from the bladder, but the sphincter muscles surrounding the urethra may not relax, inhibiting the flow of urine and leading to urinary incontinence.
Medical Conditions and Medications
Urinary incontinence can also be a side effect of certain medical conditions and medications. Chronic diseases such as diabetes, Parkinson’s disease, and dementias like Alzheimer's disease can exacerbate urinary incontinence. Furthermore, certain medications can contribute to urinary incontinence by altering the way the bladder muscle works. These include antihistamines, antispasmodics, opiates, certain types of antidepressants, blood pressure-lowering medications, antipsychotics, hormonal agents and muscle relaxants.
Additionally, surgical procedures, especially those involving the urinary tract or the pelvic area, can sometimes result in temporary or long-term urinary retention. This is often the result of anesthesia, which can temporarily impair nerve function, or due to swelling and inflammation from the surgery itself.
Lifestyle Factors and Other Causes
Lifestyle factors can also play a significant role in urinary incontinence. For example, a lack of physical activity, poor diet, unmanaged blood pressure, and obesity can all increase the risk of urinary incontinence. Another lifestyle-related cause is excessive fluid intake, which can strain the bladder and lead to incontinence.
Apart from these, restricted mobility due to conditions like arthritis or Parkinson’s disease can lead to accidents due to not reaching the bathroom in time. Also, stool impaction or severe constipation can restrict the release of urine from the bladder, causing a dribbling overflow pattern of wetting.
At ProMed DME, we believe understanding these causes is vital in managing and treating urinary incontinence effectively. In the upcoming sections, we will explore the symptoms and impact of urinary incontinence, as well as prevention and management strategies to help improve the quality of life for those suffering from this condition.
Recognizing the Symptoms and Impact of Urinary Incontinence
Understanding the symptoms of urinary incontinence is the first step towards effective management and treatment. Recognizing these signs early can make a significant difference in the quality of life for elderly individuals and their caregivers.
Symptoms of Different Types of Incontinence
Urinary incontinence can manifest in several ways, depending on the underlying cause. Here are some of the most common types and their typical symptoms:
- Urgency: This is characterized by a sudden and hard-to-ignore need to pass urine.
- Frequency: This type of incontinence involves needing to pass urine more than 8 times a day, or more than once at night.
- Stress Incontinence: Leakage of urine occurs with certain activities such as coughing, laughing, or jumping.
- Overflow Incontinence: Usually due to bladder outlet obstruction or an underactive bladder muscle. This results in an overly full bladder that leaks small amounts of urine as a constant small dribble.
- Functional Incontinence: Also known as "Disability-associated" incontinence, this occurs when getting to and using the toilet successfully is the main barrier. It is often a significant part of incontinence in people living with dementia.
- Mixed Symptoms: This involves a mixture of the above symptoms.
Moreover, acute urinary retention can present with severe discomfort or pain in the lower abdomen, an urgent need to urinate but the inability to do so, and bloating of the lower abdomen. This condition is a medical emergency and requires immediate attention.
The Impact of Urinary Incontinence on Quality of Life
Urinary incontinence can significantly impact the quality of life of older adults and their caregivers. This condition can lead to social embarrassment, anxiety, and even depression. It can also create practical challenges, such as frequent changes of clothing and bedding.
For caregivers, managing urinary incontinence can be physically and emotionally exhausting, leading to caregiver burnout. The impact of incontinence can also extend beyond the individual and caregiver to affect relationships and social interactions.
At ProMed DME, we understand the gravity of these challenges. That's why we are committed to providing a comprehensive range of high-quality urology products and services to help manage urinary incontinence. Our registered nurse can guide you on how to use your incontinence supplies safely, ensuring optimal comfort and efficacy.
Remember, urinary incontinence is not just a normal part of aging. It's a medical condition that deserves attention and care. By recognizing the symptoms and understanding the impact, we can take the first steps towards improving quality of life for our loved ones. In the following sections, we'll explore prevention and management strategies, as well as treatment options for urinary incontinence in the elderly.
Prevention and Management Strategies for Urinary Incontinence
Achieving a higher quality of life despite urinary incontinence lies in effective prevention and management strategies. Here at ProMed DME, we understand the importance of comprehensive care. This includes adopting lifestyle changes, performing specific exercises, and maintaining a healthy weight and lifestyle. Let's delve into some of these strategies.
Lifestyle Changes and Dietary Adjustments
The foundation of managing urinary incontinence lies in making certain lifestyle changes and dietary adjustments. These modifications can significantly enhance the effectiveness of your treatment and improve your overall quality of life.
For instance, a well-balanced diet plays a significant role in managing urinary retention. While there's no specific "urinary retention diet," consuming a diet rich in fiber can help prevent constipation, which, if severe, can contribute to urinary retention. Moreover, staying well-hydrated promotes healthy urine flow and prevents urinary tract infections, which can exacerbate urinary retention.
However, you should be mindful of your fluid intake and timing. Drinking too much fluid in a short time can overfill the bladder, causing discomfort if you have urinary retention. On the other hand, limiting fluid intake in the hours before bedtime can help reduce the need for nighttime urination.
Pelvic Floor Exercises and Bladder Training
In addition to diet and lifestyle changes, physical therapy, particularly pelvic floor exercises, can play a crucial role in managing urinary incontinence. A physical therapist specializing in pelvic floor problems can help stretch tight pelvic floor muscles and teach you how to keep them relaxed. This improves the efficiency of the nerves and muscles you use to empty your bladder.
Furthermore, bladder training techniques can be effective in managing urinary retention. Your healthcare provider may suggest timed voiding—urinating at set times—to prevent your bladder from becoming too full. Another technique is double voiding—waiting a short time after you urinate to try and go again. This helps ensure your bladder is completely empty after you urinate.
The Role of Weight Management and Smoking Cessation
Weight management plays a crucial role in preventing and managing urinary incontinence. Excess weight can put pressure on the bladder and surrounding muscles, leading to urinary issues. Hence, maintaining a healthy weight can help alleviate some of the symptoms of urinary incontinence.
Moreover, research has shown that quitting smoking can improve bladder health. Smoking has been linked to an increased risk of bladder cancer and can cause a chronic cough, which can lead to episodes of stress incontinence. Therefore, saying "no" to smoking can help manage some bladder issues.
To sum up, at ProMed DME, we believe that a comprehensive approach to managing urinary incontinence—one that combines medical treatment, self-care strategies, and the use of quality medical supplies—can significantly enhance treatment outcomes and improve your quality of life.
Treatment Options for Urinary Incontinence in the Elderly
Navigating the world of urinary incontinence treatments can feel like a maze, but with the right information and guidance, the path to better bladder control becomes clearer. From non-invasive techniques to surgical interventions, there's a broad spectrum of options to consider when managing urinary incontinence.
Non-Invasive Treatments: Behavioral Techniques and Medications
Among the first line of defense against urinary incontinence are behavioral techniques, which include bladder training and pelvic floor exercises. Bladder training encourages timed voiding—urinating at set times—to prevent your bladder from becoming too full. Double voiding, waiting a short time after you urinate to try again, ensures your bladder is completely empty.
Pelvic floor exercises, also known as Kegel exercises, are particularly beneficial. These exercises strengthen the muscles that hold urine in the bladder and control the flow of urine.
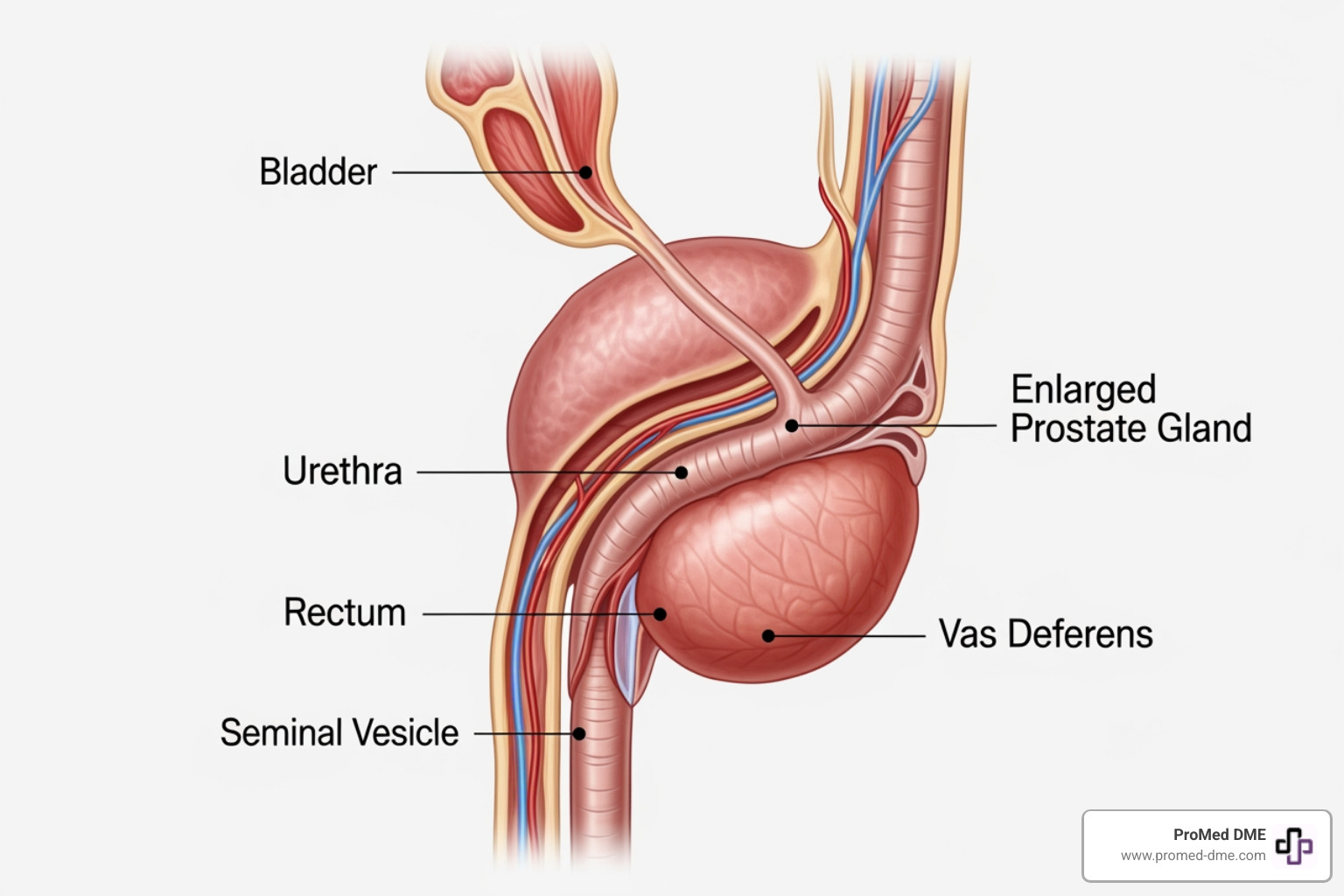
In addition to behavioral techniques, medications can also be effective. Antimuscarinics and Beta-adrenergic agonists are the two main types of medications for urge incontinence, while Alpha-1 adrenergic antagonists and 5-alpha-reductase inhibitors are often used for men experiencing overflow incontinence related to an enlarged prostate. However, medications should be used judiciously, especially in older adults, and always in conjunction with other lifestyle changes.
Invasive Treatments: Devices, Injections, and Surgery
While the idea of surgery might be daunting for some, it can be a viable option when non-invasive treatments aren't effective. For instance, women with stress incontinence can see considerable improvement or complete continence with a surgical procedure involving a mesh sling to support the urethra. Another less invasive option could be an injection of a “bulking agent” into the urethra.
However, the decision to undergo surgical intervention should be a carefully considered one, factoring in the person's overall health, mobility, and cognitive function.
The Role of Durable Medical Supplies in Managing Incontinence
At ProMed DME, we believe in the importance of quality medical supplies in managing urinary incontinence. From incontinence pads to catheters, these supplies can significantly enhance patient comfort and convenience.
We offer a range of catheter options to suit each individual's needs, including Coude catheters with a slightly curved tip designed for patients who cannot insert a straight tip catheter, and closed system catheters specifically designed to combat urinary tract infections.
In conclusion, managing urinary incontinence involves a combination of lifestyle changes, behavioral techniques, medical or surgical treatments, and the use of quality medical supplies. At ProMed DME, we're committed to supporting you every step of the way, providing the necessary medical supplies and advice to assist in your care.
Supporting an Elderly Loved One with Urinary Incontinence
Helping a loved one navigate the challenges of urinary incontinence can feel overwhelming, but you're not alone. At ProMed DME, we're here to offer expert advice and support. In this section, we'll explore how to create a supportive environment, manage incontinence in elderly parents with dementia, and advocate for proper treatment and care.
Creating a Supportive Environment
Creating a supportive environment starts with understanding and empathy. Remember, urinary incontinence can be a source of embarrassment and distress for your elderly loved one, so it's important to approach the situation with sensitivity and patience.
Start by setting up a bathroom schedule that fits their needs, aiming for regular toilet trips every two to four hours. This proactive approach can help to manage the incontinence and reduce the risk of accidents.
Consider investing in quality incontinence products. Adult diapers, incontinence pads, and protective bedding can provide comfort and confidence. At ProMed DME, we offer a wide range of durable medical supplies to assist in managing incontinence.
Managing Incontinence in Elderly Parents with Dementia
When your elderly loved one has dementia, managing incontinence can be particularly challenging. They might forget to go to the bathroom or struggle to recognize the need.
In such cases, it's helpful to establish a routine and stick to it. Scheduled toilet trips can help reduce accidents and maintain dignity. It's also important to ensure easy access to the bathroom, with clear paths and adequate lighting.
Another crucial factor is communication. Use simple, direct language to remind them about bathroom breaks and reassure them about any accidents. Patience, compassion, and understanding are key in these delicate situations.
Advocating for Proper Treatment and Care
Finally, it's crucial to advocate for your loved one's medical needs. This means seeking out the best treatment options for their specific type of urinary incontinence and working closely with healthcare providers to ensure optimal care.
Don't hesitate to ask questions or seek a second opinion if necessary. Remember, urinary incontinence is often treatable, and many seniors find relief with the right approach to care.
At ProMed DME, we're here to support you and your loved one throughout this journey. We believe that a comprehensive approach to managing urinary incontinence—one that combines medical treatment, self-care strategies, and the use of quality medical supplies—can significantly enhance treatment outcomes and improve your loved one's quality of life.
In the next section, we'll wrap up our comprehensive guide on managing elderly urinary incontinence.
Conclusion
Navigating the complex world of elderly urinary incontinence can be daunting, but the good news is that you're not alone. At ProMed DME, we understand the unique challenges that come with managing urinary incontinence in the elderly, and we are here to offer support, resources, and quality medical supplies to ease your journey.
Urinary incontinence is not just a medical issue—it's a matter that affects the quality of life, independence, and mental well-being of our elderly loved ones. As we've discussed throughout this guide, it's crucial to understand the various types and causes of urinary incontinence, recognize its symptoms, and be aware of the potential impact it can have on a person's life.
Remember, prevention and management strategies can play a significant role in dealing with this condition. It's not just about medication and surgery—lifestyle changes, dietary adjustments, bladder training, and pelvic floor exercises can all contribute to managing urinary incontinence effectively.
Treatment options are diverse and should be individualized to fit the needs and situation of the person affected. Non-invasive treatments, such as behavioral techniques and medications, can be highly beneficial. Meanwhile, more invasive treatments, like devices, injections, and surgery, can offer solutions when other methods are not enough.
Above all, the importance of quality medical supplies, such as those provided by ProMed DME, cannot be overstated. The right products can significantly enhance comfort, dignity, and independence, making a huge difference in day-to-day life.
Supporting an elderly loved one with urinary incontinence is not only about providing physical care—it's also about understanding, empathy, and ensuring their dignity. As caregivers, family members, and friends, we have a crucial role to play in creating a supportive environment and advocating for proper treatment and care.
In conclusion, managing elderly urinary incontinence might be challenging, but with the right knowledge, strategies, and support, it's a challenge we can meet head-on. At ProMed DME, we're committed to walking this path with you, providing the medical supplies you need and the support you deserve. Together, we can improve the quality of life for the elderly and those who care for them—one step at a time.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.