Pump It Up: A Deep Dive into Insulin Pump Functionality

Beyond the Syringe: Understanding Modern Diabetes Technology
How does an insulin pump work? An insulin pump is a small, computerized device that delivers rapid-acting insulin continuously through a thin tube inserted under your skin. It mimics your pancreas by providing steady background insulin (basal) 24/7 and larger doses (bolus) when you eat or need to correct high blood sugar.
Quick Answer:
- Basal delivery: Steady trickle of insulin throughout the day and night
- Bolus delivery: Larger doses for meals or blood sugar corrections
- Components: Pump device, insulin reservoir, tubing, and cannula under skin
- Control: User programs doses via pump buttons or smartphone app
For many people with diabetes, managing blood sugar is a constant balancing act. Traditional insulin injections often mean multiple daily shots and rigid meal timing. Insulin pump therapy offers a different approach, using a small, wearable device that delivers insulin automatically, like a tiny artificial pancreas working around the clock.
Today's pumps are smart devices that can integrate with continuous glucose monitors, calculate precise doses, and even adjust insulin delivery automatically. If you're tired of multiple daily injections or unpredictable blood sugars, understanding how insulin pumps work is the first step toward better diabetes management.
What is an Insulin Pump?
An insulin pump is a small computer that delivers a continuous, controlled flow of rapid-acting insulin. This wearable medical device is an alternative to injections, mimicking the pancreas to help maintain stable blood sugar levels. Its beauty lies in its precision, delivering doses to a tenth or even a hundredth of a unit—far more accurately than syringes or pens. This allows for fine-tuning your insulin intake to match your body's needs.
How is it Different from Injections?
The most immediate difference is the reduction in needle pokes. With a pump, you insert a small, flexible cannula under your skin that stays in place for two to three days. This means far fewer injections.
Pump precision also allows for more flexible living. Traditional injections often require strict meal schedules, but a pump delivers rapid-acting insulin continuously, replacing the need for long-acting insulin. This lets you eat when you want, not when your insulin dictates.
The pump also makes it easy to adjust your insulin intake for meals or exercise. This adaptability helps keep blood sugar levels stable and can improve hemoglobin A1c levels.
How Does an Insulin Pump Work? A Look at the Mechanics
Essentially, how does an insulin pump work is like having a miniature, intelligent pharmacy attached to your body, dispensing the precise amount of insulin you need, when you need it.
The pump itself, about the size of a small smartphone, clips onto your belt or tucks into a pocket. Inside, a computerized motor pushes insulin from a small reservoir through thin, flexible tubing into your body.

This system is remarkable for delivering insulin in two ways: a steady trickle of insulin (basal insulin) throughout the day and night, and extra doses (boluses) for meals or to correct high blood sugar. This dual-delivery approach closely mimics a healthy pancreas.
For comprehensive information about pump therapy, the American Diabetes Association on Insulin Pumps offers valuable insights and guidelines.
The Core Components of a Pump System
An insulin pump system is a three-part team working to keep your blood sugar stable.
The pump is the "brains" of the operation. This small, battery-powered device has a screen and buttons to program doses, review history, and adjust settings. It allows for precise dosing down to fractions of a unit, which is nearly impossible with syringes.
The reservoir or cartridge stores your insulin. This plastic container inside the pump holds enough rapid-acting insulin for two to three days, eliminating the need to carry vials.
The infusion set connects the pump to your body. It includes tubing that carries insulin and a soft cannula that sits under your skin. A tiny needle guides the cannula into place and is then removed, leaving only the comfortable tube. The set is changed every two to three days to ensure proper absorption and prevent skin issues.
How does an insulin pump work to deliver basal insulin?
Your body needs a constant supply of background insulin, called basal insulin, even when you're not eating. This keeps your blood sugar from climbing too high.
An insulin pump allows you to program different basal rates for different times of day, creating a personalized schedule that matches your body's unique patterns. You might need more insulin in the morning to combat the "dawn phenomenon" or less during a workout.
The pump delivers these tiny, programmed doses every few minutes, creating a continuous drip that mimics a healthy pancreas. Unlike fixed long-acting insulin shots, pump therapy provides incredible hour-by-hour control. This steady insulin flow prevents high blood sugars between meals and gives you flexibility.
How does an insulin pump work to deliver bolus insulin?
When you eat or need to correct high blood sugar, you use bolus insulin. These are larger, user-initiated doses that handle carbohydrates in meals or bring down high readings.
Modern pumps make this process nearly effortless. Many feature a built-in bolus calculator that considers your current blood sugar, carb intake, and any active insulin to suggest the perfect dose.
This mealtime insulin delivery offers freedom from rigid schedules. Pumps can also deliver extended boluses, which release insulin slowly over several hours—perfect for slow-digesting foods. The ability to deliver quick correction doses means you can respond immediately to high blood sugar, making diabetes management fit your life.
Types of Pumps and Integration with Modern Tech
The world of insulin pumps has evolved into multiple options designed to fit different lifestyles. Understanding these choices and how they integrate with other diabetes technologies can help you find the perfect match.
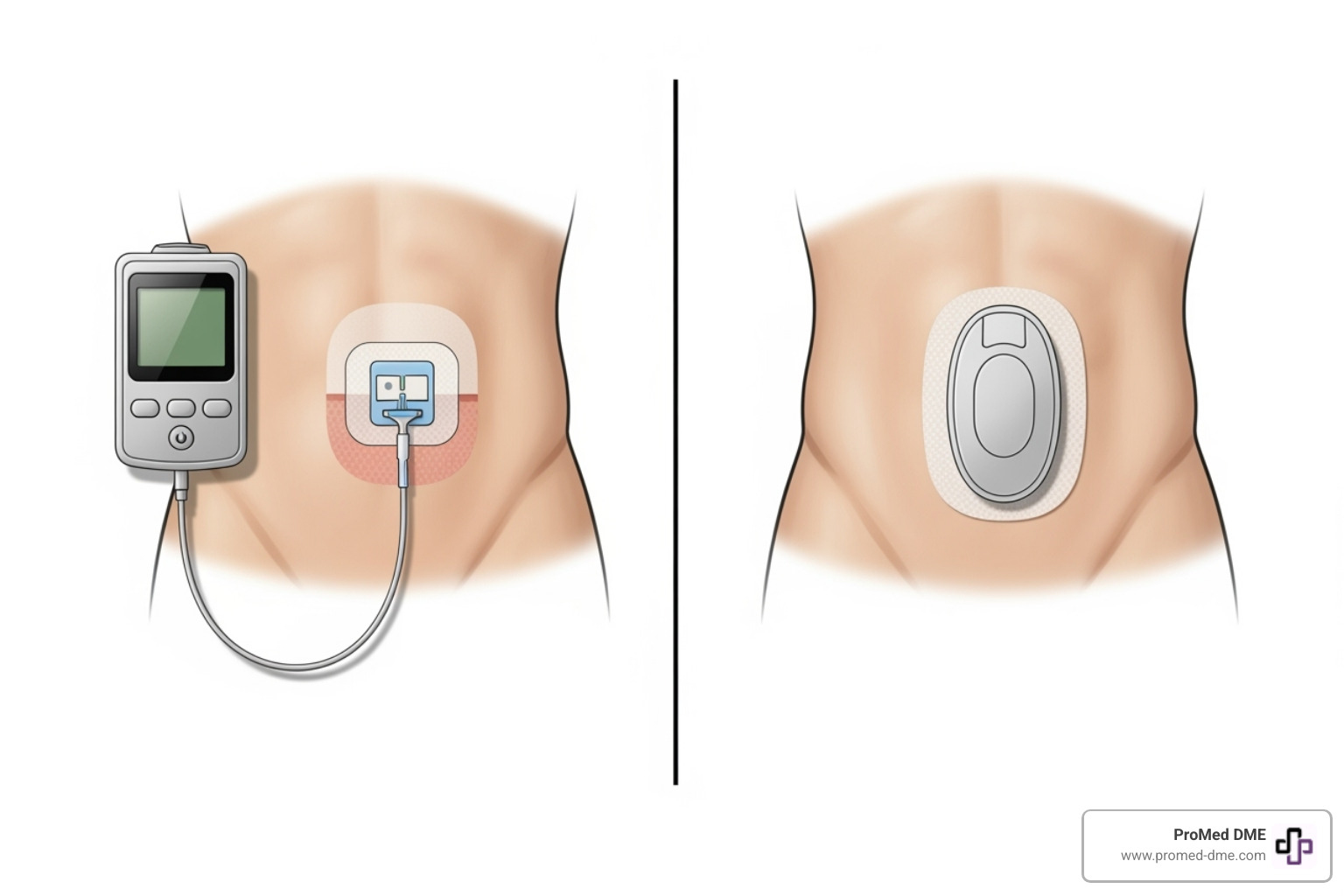
Tubed vs. Tubeless (Patch) Pumps
When exploring how does an insulin pump work, you'll find two main styles.
Traditional tubed pumps are the classic tethered system. The pump device sits separately from your body, connected by a thin tube to the cannula under your skin. You can wear it on a belt or in a pocket. The main advantage is flexibility; you can disconnect the tubing for short periods to shower, swim, or play sports without removing the cannula.
Tubeless patch pumps combine the reservoir, pump mechanism, and cannula into a single pod that sticks directly to your skin. There is no external tubing. You manage everything through a wireless remote or your smartphone, offering incredible discretion and freedom of movement. The trade-off is that patch pumps are disposable units replaced every few days, while tubed pumps only require changing the infusion set.
The Role of Continuous Glucose Monitoring (CGM)
The integration of insulin pumps with Continuous Glucose Monitoring (CGM) technology has revolutionized diabetes management.

A CGM sensor sits under your skin, measuring glucose levels continuously. Unlike single-point finger sticks, a CGM provides a constant stream of data, including trend arrows and real-time glucose data, to your pump and smartphone.
When a pump and CGM work together, they create Automated Insulin Delivery (AID) systems, also known as closed-loop systems. It's like having a personal, automated diabetes assistant.
These smart systems use algorithms to predict blood sugar trends. The pump then automatically adjusts basal insulin to keep you in your target range. Some advanced systems can even deliver small, automatic correction doses if they detect you're trending high.
This integration significantly reduces the mental burden of diabetes. The system handles many daily adjustments, helping to keep your blood sugar stable. The result is often improved time in range, fewer dangerous low blood sugars, and better overall control. If you're curious about these sensors, you can find more info about CGM supplies on our website.
The Benefits and Risks of Insulin Pump Therapy
Choosing insulin pump therapy means weighing the benefits against the challenges. For most people, the freedom and control that comes with understanding how does an insulin pump work in their daily life far outweighs the potential downsides. It's important to understand both sides of the equation.
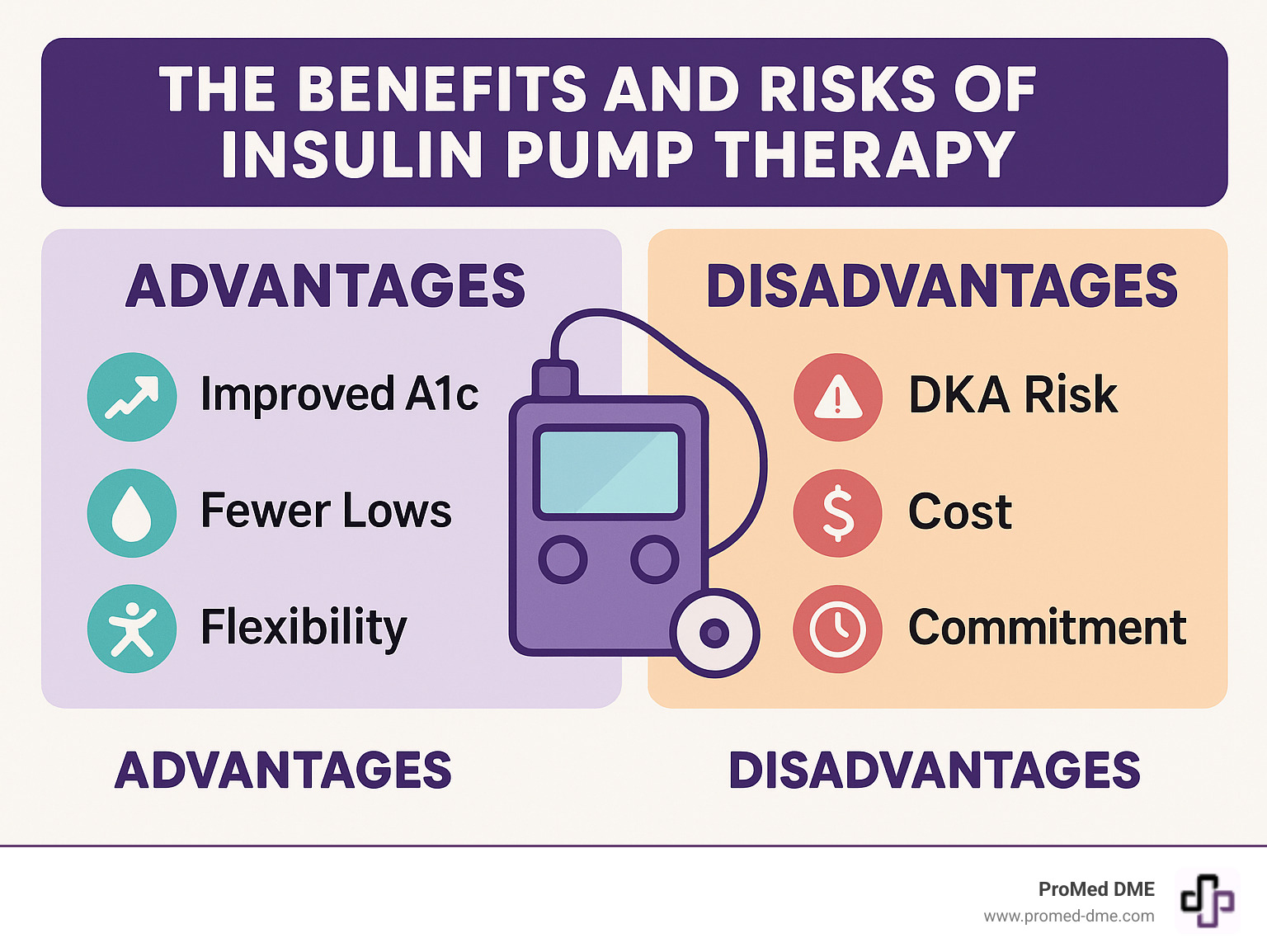
Key Advantages for Diabetes Management
Research shows insulin pumps can be game-changers for diabetes management, offering measurable and meaningful benefits.
Improved A1c levels are often seen, as studies show pump users tend to have better long-term blood sugar control than those using injections. Pump users also experience fewer severe low blood sugars. The ability to fine-tune or suspend insulin delivery reduces hypoglycemic episodes, especially during exercise or sleep.
The precise, small-dose delivery is life-changing for children or anyone highly sensitive to insulin. Dosing to a fraction of a unit eliminates the guesswork of syringes. The real freedom, however, is greater flexibility with meals and exercise. With on-demand, rapid-acting insulin, you can live on your schedule, not your insulin's.
Pumps can also manage the dawn phenomenon by delivering higher programmed basal rates in the early morning to prevent this blood sugar rise while you sleep.
Potential Drawbacks and Safety Considerations
Insulin pumps aren't magic and come with important considerations.
The most serious risk is diabetic ketoacidosis (DKA) if insulin delivery is interrupted. Since pumps use only rapid-acting insulin, a disruption from a kinked tube or malfunction can lead to DKA much faster than with injections. Users must be alert and always have backup injectable insulin.
Skin infections or irritation at the infusion site are possible. The cannula must be changed every two to three days, and proper site care is essential. Some users experience irritation from the adhesive.
The cost of the pump and ongoing supplies can be significant. While most insurance covers the pump, monthly supplies add up. Check with your insurance provider about coverage.
Pump therapy requires training and commitment. You must learn carbohydrate counting, pump programming, and troubleshooting. A pump amplifies good habits but doesn't replace them.
Like any electronic device, pumps can malfunction. Knowing how to troubleshoot and having a backup plan with injectable insulin is essential. Finally, there's the constant attachment of wearing a medical device 24/7. Most people adapt, but it's a lifestyle consideration.
Is an Insulin Pump Right for You?
Deciding to start insulin pump therapy is a key conversation to have with your healthcare team. It's a new approach to diabetes management that can transform your life. The real question is whether this technology aligns with your lifestyle, goals, and readiness for a more active role in your care.
Who is a Good Candidate for a Pump?
While every situation is unique, good candidates often share certain traits. Individuals with Type 1 diabetes are common users, but people with insulin-dependent Type 2 diabetes struggling with injections also benefit.
An active lifestyle is well-suited for a pump, as you can reduce basal insulin for exercise to prevent lows. If you crave more flexibility for travel, irregular hours, or meal timing, a pump offers significant freedom.
Those with frequent hypoglycemia find relief with a pump's precise dosing and suspension features. It's also helpful for managing the dawn phenomenon or gastroparesis.
Being comfortable with technology helps, but you don't need to be an expert. Modern pumps are user-friendly, and comprehensive training is provided.
The Process of Starting on a Pump
Starting pump therapy begins with a consultation with your endocrinologist to review your management, goals, and readiness for the commitment.
Verifying insurance coverage is next. At ProMed DME, our team steers insurance for you, working with most plans to minimize your costs and handling all verification and authorization.
Choosing the right pump means exploring different models (tubed vs. tubeless) to fit your lifestyle. Your care team will offer recommendations, and some manufacturers offer trial programs.
Comprehensive training is essential. Certified trainers will teach you everything from programming and dosing to insertion and troubleshooting. It's a vital investment in your success.
Regular follow-ups with your healthcare team are crucial, especially at first, to fine-tune your settings and optimize control.
Maintenance and Upkeep
Successful pump use requires new routines, but they quickly become second nature.
Changing your infusion set every 2-3 days is a quick, routine process where you rotate sites to prevent issues. You'll also need to refill the insulin reservoir every few days and perform infrequent battery changes.
The most important part of maintenance is having a solid backup plan. Always keep injectable insulin (pens or syringes) on hand for malfunctions or site issues. Knowing how to switch back to injections temporarily is key to safety.
Troubleshooting skills develop with time. Your training will cover common alerts like occlusions (blockages) or low battery warnings. While pump therapy requires more daily attention than injections, most users find the flexibility and improved control make it worthwhile.
Frequently Asked Questions about Insulin Pumps
We understand that switching to an insulin pump brings up practical questions. Here are the most common concerns we hear.
How painful is an insulin pump?
Most people find insulin pumps much less painful than multiple daily injections. The initial insertion is a quick poke, but the needle is immediately removed, leaving only a soft, flexible cannula under the skin.
The cannula is so comfortable that most users forget it's there. Since you only change the set every two to three days, you experience far less discomfort than with multiple daily shots. The freedom from constant needle pokes is a major quality-of-life improvement.
Can you shower or swim with an insulin pump?
This depends on the pump model. Many are water-resistant (can handle splashes), while some are fully waterproof for swimming and showering. Always check the manufacturer's guidelines.
If your pump isn't waterproof, you can disconnect most tubed pumps from the infusion set for up to an hour to shower or swim. Remember to reconnect promptly.
Patch pumps are often waterproof by design. Either way, you can maintain an active lifestyle.
How do you sleep with an insulin pump?
Sleeping with a pump is easier than most people expect, and users typically adapt within a few nights.
For tubed pumps, the long tubing allows for comfortable movement. You can clip the pump to your pajamas, put it in a pocket, or place it on the bed beside you.
Patch pumps are simpler at night as they're attached directly to your skin with no tubing to worry about.
Most users barely notice the pump during sleep after a week or two. The continuous insulin delivery can also lead to more stable overnight blood sugars and better sleep.
Your Partner in Diabetes Management
Understanding how does an insulin pump work is the first step. These remarkable devices offer more control over your blood sugar and the freedom to live life on your terms.
Switching to pump therapy is a big decision requiring education, commitment, and strong support from your healthcare team. While there's a learning curve, the potential benefits—better A1c levels, fewer low blood sugars, and incredible flexibility—are often worthwhile.
Navigating diabetes supplies, from insurance to ordering, can be overwhelming on top of daily care. That's where ProMed DME comes in. We're your partners, and our team understands the daily challenges of managing diabetes.
What sets us apart? We offer free shipping nationwide, have a dedicated nurse on staff to answer your questions, and work with most insurance plans to minimize your out-of-pocket costs. Our goal is to make managing your diabetes as easy and stress-free as possible. From insulin pump supplies to CGM sensors, we're here to support you every step of the way.
Ready to take the next step in your diabetes management journey? Learn more about our diabetes supplies and find how we can help you pump it up toward better health!
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



