Pump It Up: Understanding How Insulin Pump Therapy Functions

Why Understanding Insulin Pump Therapy Can Transform Your Diabetes Care
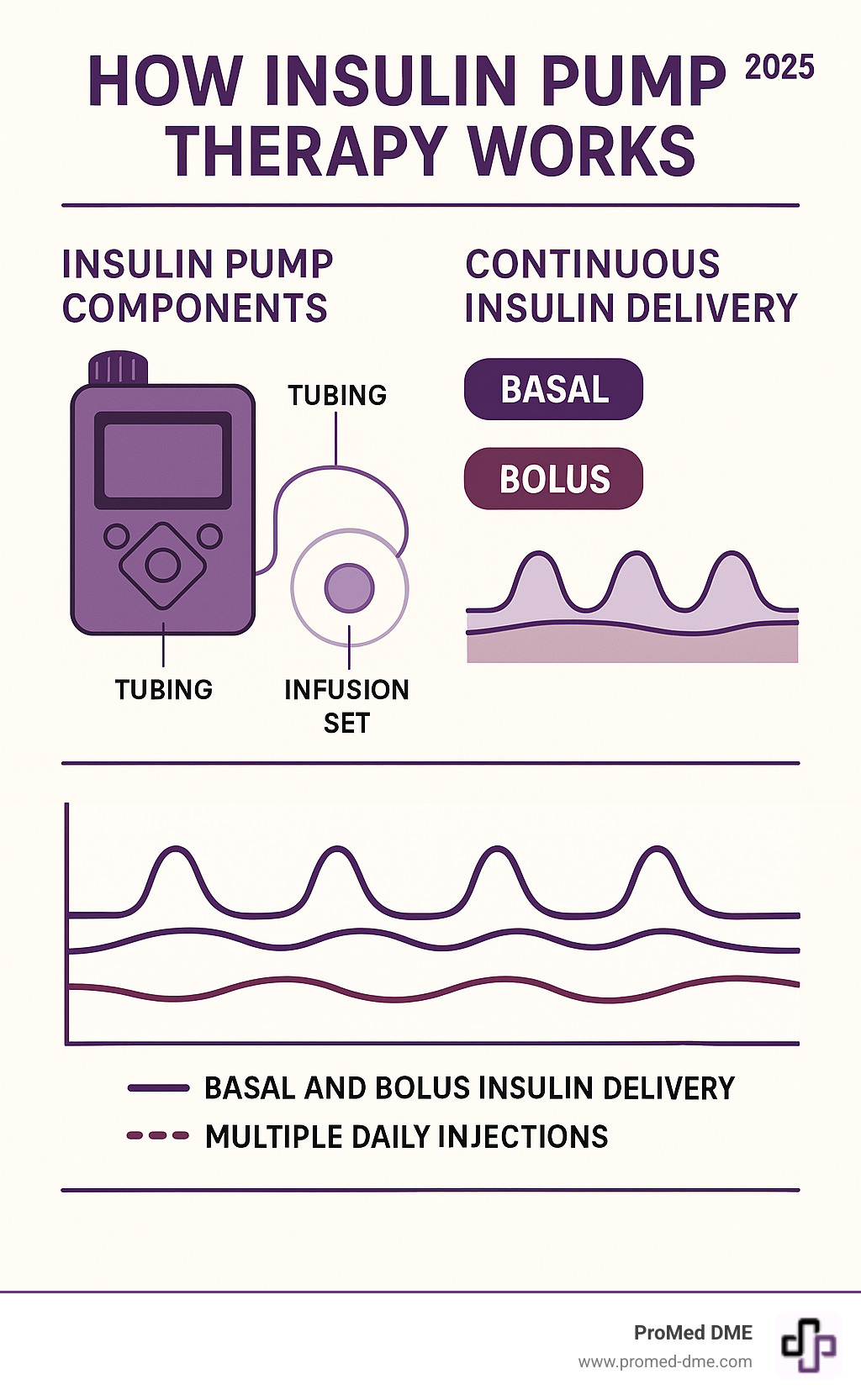
How insulin pump therapy works is simple: a small, computerized device acts like an artificial pancreas, delivering rapid-acting insulin continuously through a thin tube under your skin. This mimics a healthy pancreas by providing steady background insulin (basal) 24/7 and extra doses (bolus) for meals or to correct high blood sugar.
Quick Answer: How Insulin Pump Therapy Functions
- Continuous Delivery: Delivers small amounts of rapid-acting insulin every few minutes
- Two Types of Doses:
- Basal - steady background insulin all day
- Bolus - extra insulin for meals and corrections
- Precise Control: Can deliver insulin in increments as small as 0.025 units
- Programmable: Multiple basal rates throughout the day to match your body's needs
If you're tired of multiple daily injections or struggling with blood sugar control, pump therapy could be a game-changer. Studies show it can improve A1C levels by about 0.5% and reduce severe low blood sugar episodes by 40-50%. This precise delivery means more freedom around meals, exercise, and daily activities, offering a simpler way to manage insulin, especially for those with complex schedules.
Relevant articles related to how insulin pump therapy works:
- continuous glucose monitoring system
- advantages and disadvantages of insulin pump therapy
- how to use insulin pump therapy
How Insulin Pump Therapy Works: A Closer Look at the Mechanics
An insulin pump is a small, wearable computer that constantly calculates and delivers the precise amount of rapid-acting insulin your body needs. Unlike multiple daily injections with fixed doses, pump therapy mimics the natural function of a pancreas. It delivers insulin directly into the fatty tissue under your skin, allowing for much faster adjustments than long-acting insulin. This results in smooth, consistent insulin delivery that matches your body's changing needs, avoiding the peaks and valleys common with injections.

The Core Components of an Insulin Pump System
To understand how insulin pump therapy works, let's look at its three main parts.
- The pump device, about the size of a small phone, houses the motor, computer, and controls.
- The insulin reservoir is a refillable cartridge holding several days' worth of rapid-acting insulin.
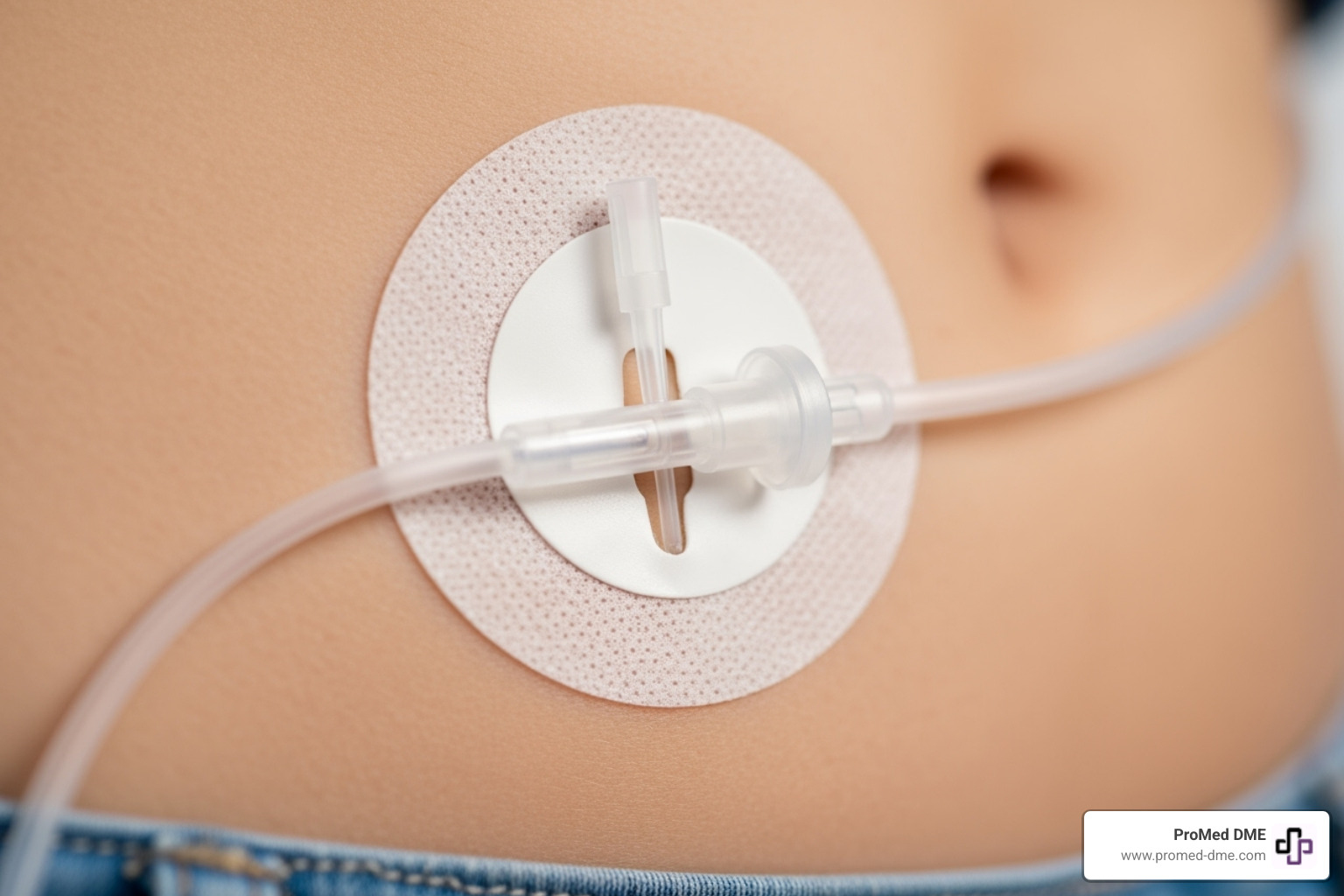
- The infusion set connects the pump to your body with thin, flexible tubing leading to a soft cannula under your skin, held by an adhesive patch. This set is typically changed every two to three days.
Understanding Basal Rates: How Insulin Pump Therapy Works Around the Clock
Your body needs a constant supply of background insulin, known as basal insulin. With injections, this is a fixed dose. How insulin pump therapy works for basal delivery is far more precise. The pump delivers tiny, programmable amounts of insulin 24/7, with precision dosing as low as 0.01 units per hour.
You and your healthcare team can set different basal rates for different times of day to counteract the dawn phenomenon or adjust for exercise. The pump automatically handles these programmable rates, covering your background insulin needs while you live your life.
Mastering Bolus Doses: How Insulin Pump Therapy Works for Meals and Corrections
Bolus insulin covers meals and corrects high blood sugar. This is where how insulin pump therapy works offers incredible flexibility. For mealtime coverage, you can eat when you want; simply enter your carbs, and the pump's bolus calculator determines the dose based on your insulin-to-carb ratio.
If your blood sugar is high, it adds a correction factor dose, accounting for any active insulin to prevent stacking. The precision dosing (as little as 0.025 units) is ideal for children or those sensitive to insulin. For high-fat or high-protein meals, an extended bolus can deliver insulin gradually over several hours.
The Pros and Cons: Weighing the Benefits and Risks of Pump Therapy
Deciding on pump therapy involves weighing its benefits against its challenges. For most, understanding how insulin pump therapy works reveals advantages that offer incredible freedom and control in exchange for some initial complexity.

Key Benefits of Insulin Pump Use
The benefits of pump therapy are often life-changing. Key advantages include:
- Fewer injections: You only change your infusion set every 2-3 days, replacing multiple daily shots.
- Precise dosing: The pump delivers insulin in tiny, programmable increments, impossible with pens or syringes, allowing for fine-tuned management.
- Improved A1C levels: This precision often leads to a significant drop in A1C (around 0.5% or more), reducing long-term complication risks.
- Reduced severe hypoglycemia: The steady insulin delivery helps prevent dangerous low blood sugar episodes, with research showing a 40-50% reduction in severe lows.
- Greater flexibility with meals and exercise: You can eat when you want, sleep in, or adjust insulin for physical activity without being tied to a rigid injection schedule. This freedom extends to travel, work, and social life.
Potential Drawbacks and Safety Considerations
It's also important to consider the potential challenges:
- Risk of Diabetic Ketoacidosis (DKA): Since pumps only use rapid-acting insulin, any interruption in delivery (e.g., a kinked tube) can quickly lead to DKA. A backup plan with insulin pens is essential.
- Infusion site issues: Skin irritation or infection can occur. Proper care, including rotating sites every 2-3 days, is crucial.
- Cost and insurance coverage: Pumps and supplies can be expensive. At ProMed DME, we help steer insurance to minimize your costs.
- Constant attachment to a device: Being connected to a device 24/7 takes getting used to, though most users adapt quickly.
- Learning curve: Mastering the pump, carb counting, and troubleshooting requires commitment and training from your healthcare team.
- Technical malfunctions: Like any electronic device, pumps can fail. Always have a backup plan.
Despite these points, most users find the improved quality of life and blood sugar control make pump therapy a worthwhile choice.
Is an Insulin Pump Right for You? Candidates and Choices
Deciding if an insulin pump is right for you is a personal choice based on your goals, motivation, and readiness to take an active role in your diabetes management. It's not a permanent commitment, and working with your healthcare team is key to determining if it's a good fit.

Who is a Good Candidate for Insulin Pump Therapy?
Good candidates for pump therapy often include:
- People with Type 1 diabetes who struggle with A1C targets, frequent low blood sugar, the dawn phenomenon, or simply want more lifestyle flexibility.
- People with insulin-requiring Type 2 diabetes who take multiple daily injections but still have poor control. Pumps can simplify their regimen and significantly improve A1C.
- Motivated individuals who are willing to monitor their glucose, count carbohydrates, and learn to use the technology.
- Those with specific lifestyle needs, such as athletes, people with irregular schedules, or women planning a pregnancy, who can benefit from the pump's adaptability.
Your healthcare team can help you figure out if you're ready to make the leap.
Tubed vs. Tubeless: Understanding Your Pump Options
If you opt for a pump, you'll choose between two main types:
- Traditional tubed pumps consist of a device (carried in a pocket or on a belt) connected to your body by thin tubing. They often have larger insulin reservoirs and can be disconnected for short periods (e.g., for showering or swimming). The main drawback is managing the tubing.
- Tubeless patch pumps are all-in-one devices that stick directly to your skin and are controlled wirelessly. They offer freedom from tubing and are often waterproof, but may hold less insulin and require more frequent changes.
| Feature | Tubed Insulin Pumps | Tubeless Insulin Pumps (Patch Pumps) |
|---|---|---|
| Components | Separate pump device, tubing, infusion set | All-in-one pod attached to skin |
| Wearability | Carried in pocket, clipped to belt, worn in pouch | Adheres directly to skin |
| Discretion | Can be discreetly tucked away, but tubing is visible | Highly discreet, no visible tubing |
| Water Resistance | Varies by model; many are water-resistant but not fully waterproof for prolonged immersion | Many are fully waterproof for continuous wear during water activities |
| Control | Buttons/touchscreen on pump device | Wireless controller or smartphone app |
| Insulin Capacity | Generally larger reservoirs (up to 300 units) | Generally smaller pods (e.g., 200 units) |
| Disconnection | Can be disconnected for short periods | Typically no disconnection needed due to waterproof design |
There is no single "best" choice—only what works for your lifestyle. Your diabetes educator can help you weigh the pros and cons. Both options deliver the core benefits of how insulin pump therapy works: better control and more flexibility.
The Next Generation: Pumps, CGMs, and Automated Insulin Delivery
The way how insulin pump therapy works is rapidly evolving. Modern systems integrate insulin pumps with Continuous Glucose Monitors (CGMs), creating smart systems that function much like an artificial pancreas. These technologies communicate to keep your blood sugar in range with less manual effort.

The Role of Continuous Glucose Monitoring (CGM)
A Continuous Glucose Monitor (CGM) uses a small sensor under the skin to measure glucose levels every few minutes. This provides:
- Real-time glucose data and trend arrows showing where your levels are heading.
- High and low alerts to warn you of potential problems, providing a crucial safety net.
- A reduction in the need for fingersticks.
- The ability to track time in range, a key metric for diabetes control.
When paired with a pump, this creates a Sensor Augmented Pump that displays CGM data directly on the pump screen, enabling smarter dosing decisions.
The Future is Now: Automated Insulin Delivery (AID) Systems
Automated Insulin Delivery (AID) systems, also known as hybrid closed-loop systems, are a major leap forward. A smart control algorithm uses CGM data to predict future glucose levels and automatically adjust insulin delivery. Key features include:
- Predictive low-glucose suspend: The system stops insulin delivery before a low occurs, significantly reducing hypoglycemia, especially overnight.
- Auto-correction boluses: Some systems can deliver small, automatic correction doses for rising blood sugar.
- Algorithm-based adjustments: The system constantly fine-tunes background insulin delivery.
These systems are "hybrid" because you still need to bolus for meals. However, they significantly increase time in range, improve A1C, and provide incredible peace of mind. It's the closest technology we have to a cure, and it's available now through scientific research on automated insulin delivery.
Frequently Asked Questions about Insulin Pump Therapy
We know you have questions about how insulin pump therapy works. Here are answers to some of the most common ones.
How does insulin pump therapy work for people with Type 2 diabetes?
Insulin pumps are an excellent option for many people with Type 2 diabetes, especially those on multiple daily injections or with poor glycemic control. How insulin pump therapy works is the same for Type 2 as for Type 1: it provides continuous basal insulin and bolus doses for meals. The benefits for Type 2 include:
- Better control: Pumps can deliver large or small insulin amounts precisely, often leading to A1C drops of a full percentage point or more.
- Fewer low blood sugars: The precision of a pump reduces the risk of hypoglycemia compared to high-dose injections.
- Flexibility: Pumps allow freedom around meal timing and lifestyle that injections don't.
Newer, user-friendly pumps are being developed specifically for the Type 2 diabetes community.
What is the process for starting on an insulin pump?
Starting on a pump is a structured process:
- Consultation: Discuss your goals, lifestyle, and motivation with your endocrinologist to see if a pump is a good fit.
- Pump Selection: Your healthcare team will help you choose between tubed and tubeless models based on your needs.
- Insurance and Supplies: ProMed DME helps steer insurance coverage to minimize your out-of-pocket costs and handles the paperwork for your pump and supplies.
- Training: A certified pump trainer will teach you everything from inserting infusion sets to programming doses and troubleshooting.
- Fine-Tuning and Support: Your healthcare team will help you adjust your settings over the first few weeks and provide ongoing support to ensure your success.
What are the most important safety practices for using an insulin pump?
Key safety practices are crucial for successful pump use:
- Rotate infusion sites: Change your site every 2-3 days to prevent infection, scar tissue, and poor insulin absorption.
- Have a backup plan: Always keep insulin pens or syringes available in case of pump failure or a site issue.
- Monitor your body and your pump: Pay attention to unexplained high blood sugar, which could signal a problem like a kinked tube. Check for pump alarms and know what they mean.
- Check blood sugar regularly: Use a CGM or fingersticks to monitor your glucose levels and catch problems early.
- Stay in touch with your healthcare team: Don't hesitate to contact your diabetes team with questions or concerns. They are your best resource for troubleshooting.
Conclusion: Taking Control of Your Diabetes Journey
Understanding how insulin pump therapy works puts you in the driver's seat of your diabetes management. Instead of rigid injection schedules, a smart device delivers precise amounts of insulin 24/7, providing both background basal insulin and mealtime bolus doses. We've covered the benefits, from fewer injections and better A1C levels to greater lifestyle freedom, as well as the challenges.
Modern automated insulin delivery systems are bringing us closer than ever to a functional artificial pancreas by using CGM data to make automatic adjustments. Whether you have Type 1 or insulin-requiring Type 2 diabetes, pump therapy could be the game-changer you need. The key is having the right support.
At ProMed DME, our dedicated nurse and experienced team are here to help with everything from navigating insurance to getting your ongoing supplies. We believe managing diabetes is about living your life on your terms. If you're considering a pump, you don't have to do it alone. We work with most insurance plans, offer free nationwide shipping, and provide the personal support that makes a difference.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.