Which Insulin Pump Wins? Your Ultimate Comparison Chart

Why Finding the Right Insulin Pump Matters for Your Daily Life
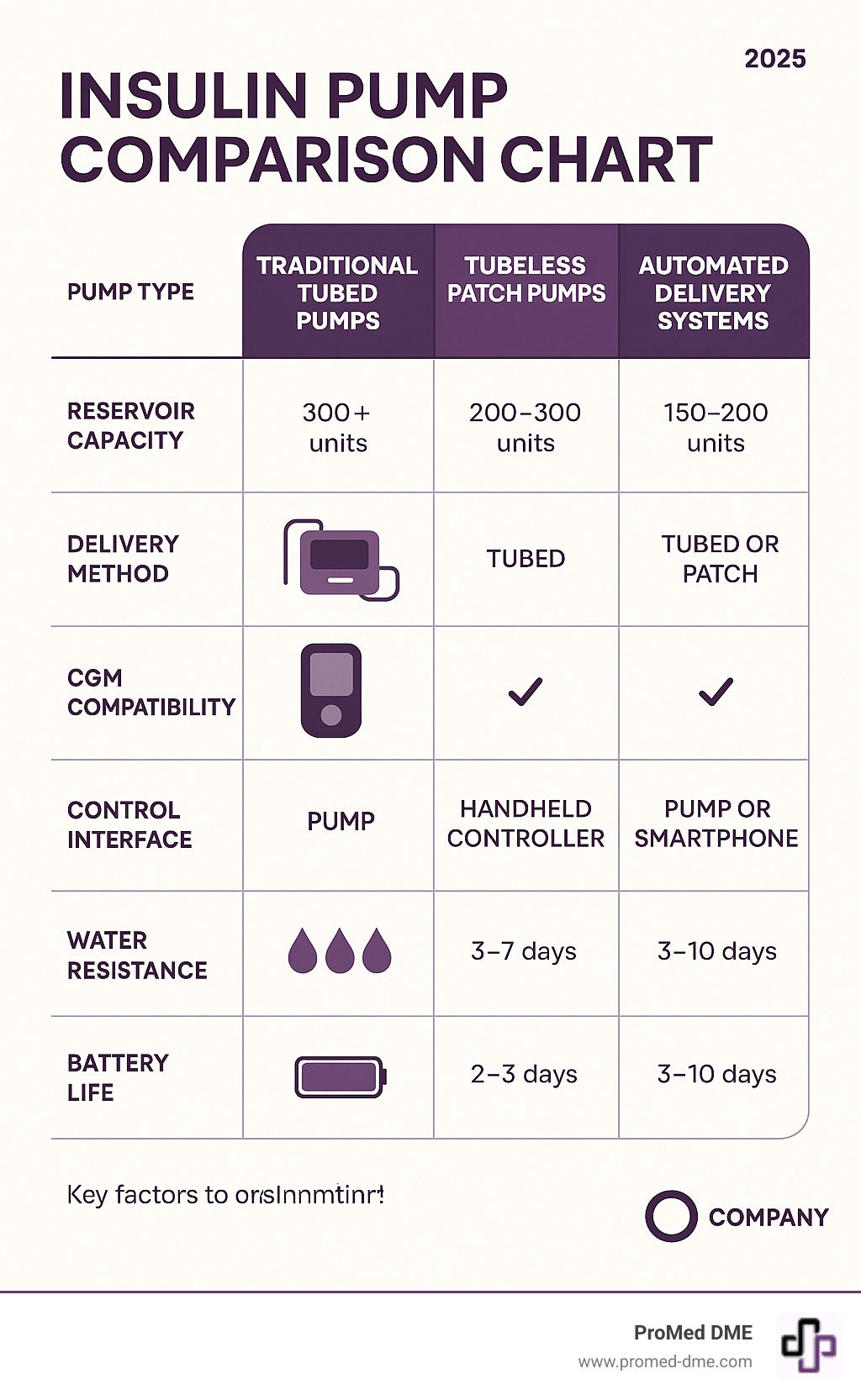
An insulin pump comparison chart helps you understand the key differences between modern diabetes management systems so you can choose the device that fits your lifestyle best. With multiple manufacturers offering everything from traditional tubed pumps to smartphone-controlled systems, making the right choice can feel overwhelming.
Here are the main types of insulin pumps to compare:
- Traditional Tubed Pumps - Larger reservoirs (300+ units), established technology, quick-disconnect options
- Tubeless Patch Pumps - No tubing to snag, increased discretion, simpler application
- Hybrid Closed-Loop Systems - Automated insulin adjustments, CGM integration, predictive technology
- Smartphone-Controlled Pumps - App-based control, remote software updates, data sharing capabilities
The right pump depends on your insulin needs, lifestyle preferences, and comfort with technology. Some people prioritize discretion and choose tubeless systems. Others want the largest possible insulin capacity or the most advanced automation features.
Key factors to evaluate include insulin delivery precision (basal rates as low as 0.01 units/hour), water resistance ratings (some tested to 8 feet), battery life (3 days to 4 weeks), and compatibility with continuous glucose monitors from Dexcom or FreeStyle Libre.
Real users report significant improvements - with some achieving 74% time in optimal glucose range after switching to automated systems. The technology has advanced dramatically, with pumps now smaller than a deck of cards and algorithms that predict glucose levels 30 minutes ahead.
Key Factors to Consider When Choosing an Insulin Pump

Finding the right insulin pump means matching a device to how you live. When creating your insulin pump comparison chart, remember the best pump isn't the one with the most features, but the one that fits your life. The three main areas to consider are insulin delivery precision, smart technology, and daily usability. Let's explore these to help you make a confident choice.
Insulin Delivery Precision
Insulin delivery precision is key for good results.
Basal rates are your background insulin. Modern pumps are very precise, with some delivering as little as 0.01 units per hour, which is ideal if you're sensitive to insulin or need small doses.
Bolus types offer flexibility. A standard bolus delivers insulin at once for most meals. An extended bolus spreads it out for slow-digesting foods like pizza. A multiwave bolus combines both.
Reservoir capacity varies from 200 to 480 units. A larger reservoir means fewer refills if you use a lot of insulin.
Temporary basal rates let you adjust background insulin for exercise or illness. Most pumps also include bolus calculators that recommend a dose based on your carbs and blood sugar, simplifying mealtime math.
Smart Technology and Connectivity
Automated Insulin Delivery (AID) systems are a game-changer. These "hybrid closed-loop" systems work with your continuous glucose monitor (CGM) to automatically adjust insulin all day.
CGM compatibility is crucial because it provides the real-time data for the system to make better decisions. The Benefits of Interstitial Fluid Measurement show how valuable this is.
Smartphone app control lets you bolus discreetly from your phone, and some pumps are controlled entirely via an app, making the device itself very small.
Remote software updates keep your pump current, while data sharing lets you easily share information with your healthcare team or family for more productive visits and peace of mind.
Daily Life and Usability
Here's how a pump works with your real life.
Water resistance is important. Ratings range from splash protection to being submersible in 8 feet of water for 2 hours, allowing you to swim or shower without worry.
Battery life varies greatly. Some pumps use disposable AA batteries that last for weeks, while others have rechargeable batteries needing a charge every few days. Some offer convenient wireless charging.
Size and weight affect comfort. The smallest pumps weigh about an ounce, while larger ones might offer more features.
Screen type ranges from full-color touchscreens to simpler displays with physical buttons, depending on your comfort with technology.
Alarms and alerts warn you about important issues. The ability to customize them (vibrate, quiet, loud) makes a big difference in daily comfort.
Tubed vs. Tubeless Pumps: Which is Right for You?
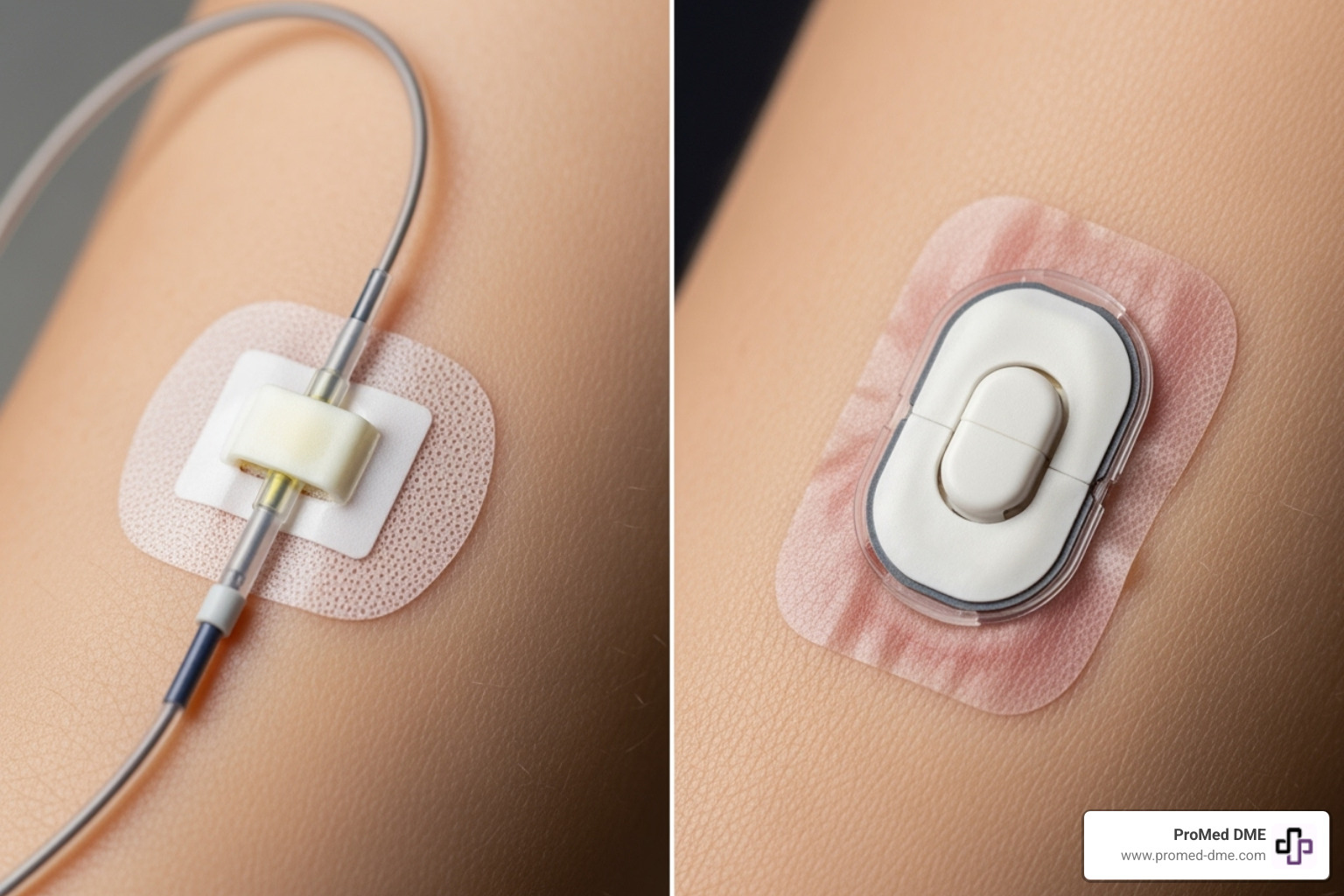
A key decision on any insulin pump comparison chart is tubed vs. tubeless. The choice depends on your lifestyle and personal preference. Tubed pumps have a main device connected to your body by thin tubing and an infusion set, which can be carried in a pocket or on a belt. Tubeless patch pumps are self-contained pods that stick directly to your skin.
Your daily activities are a major factor. Active individuals may prefer a tubeless system to avoid snagging tubes, while others might prioritize the larger insulin capacity and infusion site flexibility of a tubed pump.
Advantages of Traditional Tubed Pumps
Traditional tubed pumps have been a popular choice for decades for several key reasons.
Larger reservoir capacity is a major advantage. Many tubed pumps hold 300 to 480 units of insulin, meaning fewer changes for those with high insulin needs.
The wider variety of infusion sites offers flexibility. The separation of the pump and infusion site allows for more placement options and easier site rotation, which is crucial for skin health.
Established technology means these pumps have been refined for years, offering a wide range of infusion set options to suit different needs.
The quick disconnect feature allows you to easily disconnect the tubing for activities like showering or swimming without removing the infusion set.
Advantages of Tubeless "Patch" Pumps
Tubeless patch pumps contain everything in one small pod that adheres to your skin.
No tubing to snag is a life-changing feature for many, eliminating tangles and accidental pulls during sleep or daily activities.
Increased discretion comes from the low-profile pods that are nearly invisible under clothing.
Freedom during physical activity makes these pumps ideal for athletes and active people, as there's no external device to get in the way.
The simple application process streamlines site changes, as the all-in-one pod design includes a built-in insertion mechanism.
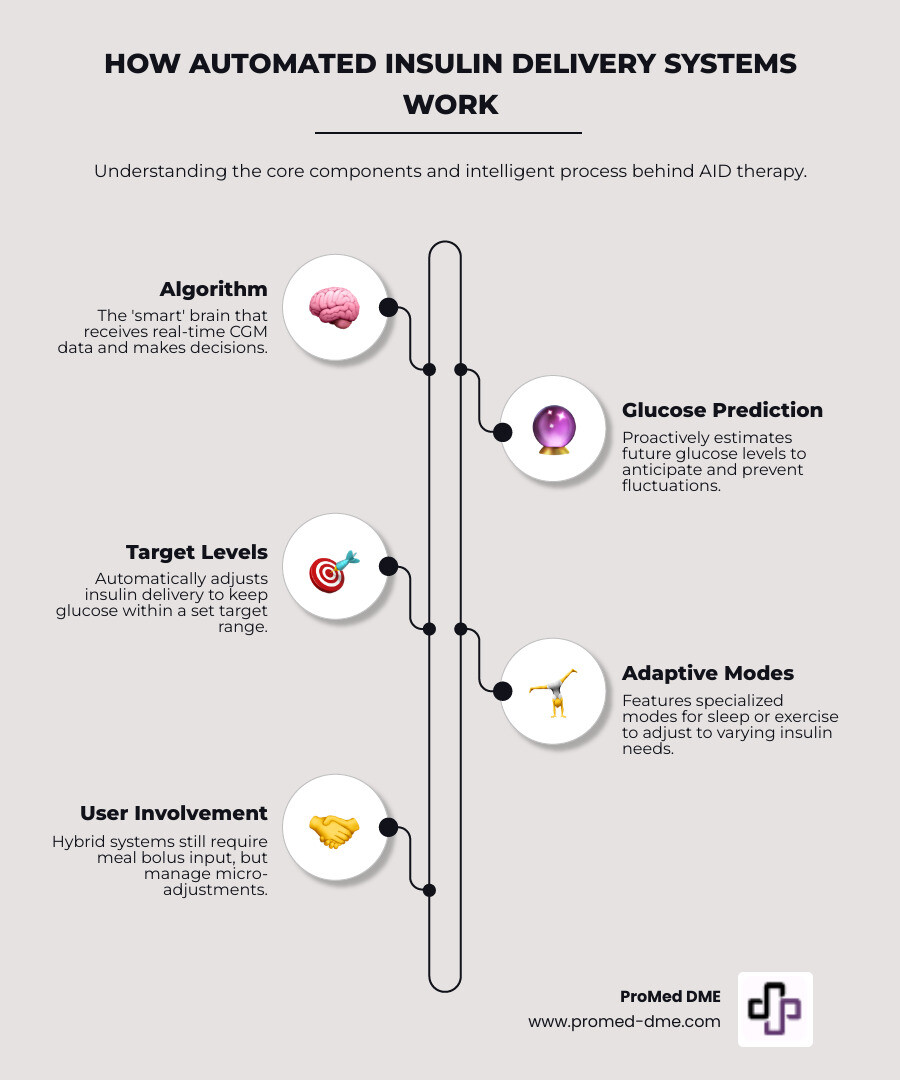
The Next Generation: Understanding Automated Insulin Delivery (AID)

Automated Insulin Delivery (AID) systems act like a personal diabetes assistant, representing the closest thing to an artificial pancreas. They reduce the burden of constant decision-making, allowing you to focus on your life.
The most common type, hybrid closed-loop systems, partners with a CGM to make predictive low-glucose suspend decisions and deliver automatic correction boluses. On any insulin pump comparison chart, AID systems show the best time-in-range results, with users often achieving 74% or more in their target zone, a result validated by scientific research on automated insulin delivery.
How AID Systems Work
A sophisticated algorithm is the brain of an AID system. It analyzes CGM data to predict glucose levels 30 to 60 minutes ahead, allowing it to proactively adjust insulin delivery.
You set your target glucose levels (e.g., 100-180 mg/dL), and the algorithm works to keep you in that range. Special modes for sleep and exercise adjust targets for different situations, like preventing lows during physical activity.
User involvement is still necessary. You must announce meals by entering carb counts for the system to calculate a bolus. It's a partnership: the system handles micro-adjustments while you manage meals.
Benefits of an Automated System
The benefits of AID systems extend beyond better glucose numbers.
Improved glycemic control means users spend more time in their target range and experience fewer highs and lows.
Reduced hypoglycemia is a major safety benefit. The system's predictive algorithm can reduce or stop insulin to prevent lows.
Reduced diabetes burden comes from the system handling micro-adjustments, which means less mental math and constant monitoring for users and their families.
More flexibility in daily life is possible because the system adapts to changes in your routine, like late meals or spontaneous exercise.
For detailed information about the continuous glucose monitors that make these systems possible, check out more info about continuous glucose monitors. These devices are the eyes and ears of your AID system.
Your Complete Insulin Pump Comparison Chart
This insulin pump comparison chart guide organizes the key technical specs and features into easy-to-digest sections. Think of it as your cheat sheet for pump shopping, focusing on the main categories to help you see the big picture.
Technical Specifications: An Insulin Pump Comparison Chart
These technical specs directly impact your daily routine and insulin management.
Insulin capacity varies across pump types. Traditional tubed pumps often hold 300 to 480 units, meaning fewer changes. Tubeless patch pumps typically hold around 200 units, while hybrid systems are often between 200 to 300 units.
Minimum basal rates can be as low as 0.01 units per hour, and bolus increments as small as 0.01 units. This precision is crucial for insulin-sensitive users or those needing small doses.
Water resistance ratings vary. Most pumps handle everyday exposure, but some are highly resistant, with ratings like an IP28 rating tested to 8 feet for 2 hours.
Battery life differs by design. Pumps using AA or AAA batteries might last a month, while rechargeable systems need charging every 3 to 5 days. Some offer wireless charging.
Most pumps come with a 4 to 5-year warranty.
Smart Features: An Insulin Pump Comparison Chart
Smart features are what separate modern pumps from older devices.
CGM compatibility is now standard, but the quality of integration varies. The best systems use real-time CGM data to inform insulin decisions automatically.
Closed-loop capability is a major leap forward. These hybrid systems predict blood sugar trends and make micro-adjustments to keep you in range.
Remote bolus capability allows for convenient and discreet dosing from a smartphone.
Software updates can improve your pump's algorithm and add features over time without you needing to buy a new device.
Data management software creates detailed reports to help you and your healthcare team identify patterns and refine your management.
A detailed insulin pump comparison chart helps you weigh which of these features matter most to you, whether it's insulin capacity or wireless charging.
Frequently Asked Questions about Insulin Pumps
When you're considering an insulin pump, it's natural to have questions. We've heard these same concerns from hundreds of families over the years, and we're here to give you straight answers that help you make the best decision for your situation.
What is the approved age for using an insulin pump?
The FDA approval age varies significantly depending on which pump you're looking at. Some systems are approved for children as young as 2 years old, while others require users to be at least 6, 7, or even 14 years old before they can use the device safely.
For example, several popular systems have FDA approval for ages 6 and up, though some doctors may recommend off-label use for younger children under very close medical supervision. The age restrictions exist because younger children have different insulin needs, smaller bodies, and may not be able to communicate pump-related issues effectively.
The key is talking with your healthcare team about which pumps are appropriate for your specific age group. Your doctor will consider factors like your child's maturity level, ability to understand pump management, and overall diabetes control when making recommendations.
How much do insulin pumps and supplies cost without insurance?
Let's be honest - insulin pumps represent a significant investment, and understanding the costs upfront helps you plan better. Without insurance coverage, you're looking at several thousand dollars for the pump itself, plus ongoing supply costs that add up throughout the year.
The initial pump cost typically ranges from about $6,300 to nearly $10,000, depending on the system you choose. Tubed pumps might cost around $7,000 to $7,400, while some of the newest smartphone-controlled systems can have list prices approaching $10,000.
But the pump is just the beginning. Annual supply costs can range from $3,000 to $3,600 without insurance coverage. These supplies include infusion sets (about $110 for a 30-day supply), insulin cartridges or pods (around $50 for ten cartridges), and replacement batteries when needed.
Here's the good news: most people don't pay these full prices. At ProMed DME, we work with most insurance plans to minimize your out-of-pocket expenses. Many insurance plans cover insulin pumps as durable medical equipment, significantly reducing what you'll actually pay.
Additionally, pump manufacturers often offer patient assistance programs and flexible payment options. You can explore resources like pump benefit programs to find potential cost-saving opportunities that make pump therapy more accessible.
Do all insulin pumps work with a Continuous Glucose Monitor (CGM)?
This is where things get a bit technical, but it's an important distinction to understand. Not all pumps work with all CGMs, and the level of integration varies significantly between different systems.
Integrated systems represent the gold standard - these are the hybrid closed-loop systems where your pump and CGM talk directly to each other. The pump automatically adjusts your insulin based on your CGM readings, creating that "artificial pancreas" effect we discussed earlier. However, these systems typically require a specific CGM model to work properly.
Standalone pumps might be "CGM compatible," meaning they can receive and display your glucose data, but they won't automatically adjust your insulin. You'll still see your numbers, but you'll need to make manual decisions about basal rate changes or correction boluses.
The connection between your CGM and pump typically happens through Bluetooth communication, creating a seamless wireless data flow. Some systems might require manual entry of glucose values for certain functions like bolus calculations, even when they're technically CGM compatible.
When you're comparing options using an insulin pump comparison chart, make sure to verify the specific CGM compatibility for any system you're considering. This ensures you'll get the level of automation and integration that matches your diabetes management goals.
Making Your Choice with Confidence
Choosing an insulin pump is a deeply personal decision that goes far beyond comparing technical specifications. There's no single "best" pump in the world – there's only the best pump for you. We understand that navigating through all the options in an insulin pump comparison chart can feel overwhelming, but remember, you don't have to make this journey alone.
Think of selecting your insulin pump like choosing a life partner (okay, maybe that's a bit dramatic, but you get the idea!). This device will be with you through thick and thin, supporting your health goals while adapting to your unique lifestyle. The key is finding that perfect match.
Lifestyle alignment should be your North Star when making this decision. Ask yourself honest questions about your daily routine. Are you constantly on the go, playing sports, or swimming regularly? A tubeless patch pump might be your best friend. Do you prefer having complete control over every setting, or would you rather let smart technology handle the micro-adjustments? These preferences will guide you toward the right choice.
Your technology comfort level plays a huge role too. Some people love the idea of controlling their pump through their smartphone – it feels natural and discreet. Others prefer the reliability and simplicity of a dedicated device with physical buttons. Neither approach is wrong; it's all about what makes you feel confident and comfortable.
Insulin needs vary dramatically from person to person. If you require large amounts of insulin daily, that 480-unit reservoir capacity might be a game-changer for you. If you're highly insulin-sensitive and need those precise 0.01-unit increments, certain pumps will serve you better than others. Your body's requirements should heavily influence your decision.
Don't forget about the practical side – cost and ongoing support. While insurance typically covers most expenses, understanding your potential out-of-pocket costs helps you plan ahead. More importantly, consider the level of customer support and educational resources available. You want a company that stands behind their products and helps you succeed.
We always recommend having detailed conversations with your healthcare team. Your endocrinologist, certified diabetes educator, or diabetes care and education specialist knows your medical history and can provide personalized guidance that no comparison chart can match. If you need help finding a qualified professional near you, the ADCES finder tool is an excellent resource.
At ProMed DME, we believe that managing diabetes well shouldn't mean compromising on the life you want to live. We're here to support you every step of the way with free shipping, a dedicated nurse on staff to answer your questions, and our commitment to working with most insurance plans to keep your costs manageable.
Ready to take the next step in your diabetes management journey? We'd love to help you explore your options and find the perfect pump for your unique needs. Contact us to discuss your diabetes supply needs – because you deserve both excellent health and the freedom to live life on your terms.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



