External Catheters Uncovered! Medicare Coverage Explained

Medicare's External Catheter Coverage: What You Need to Know
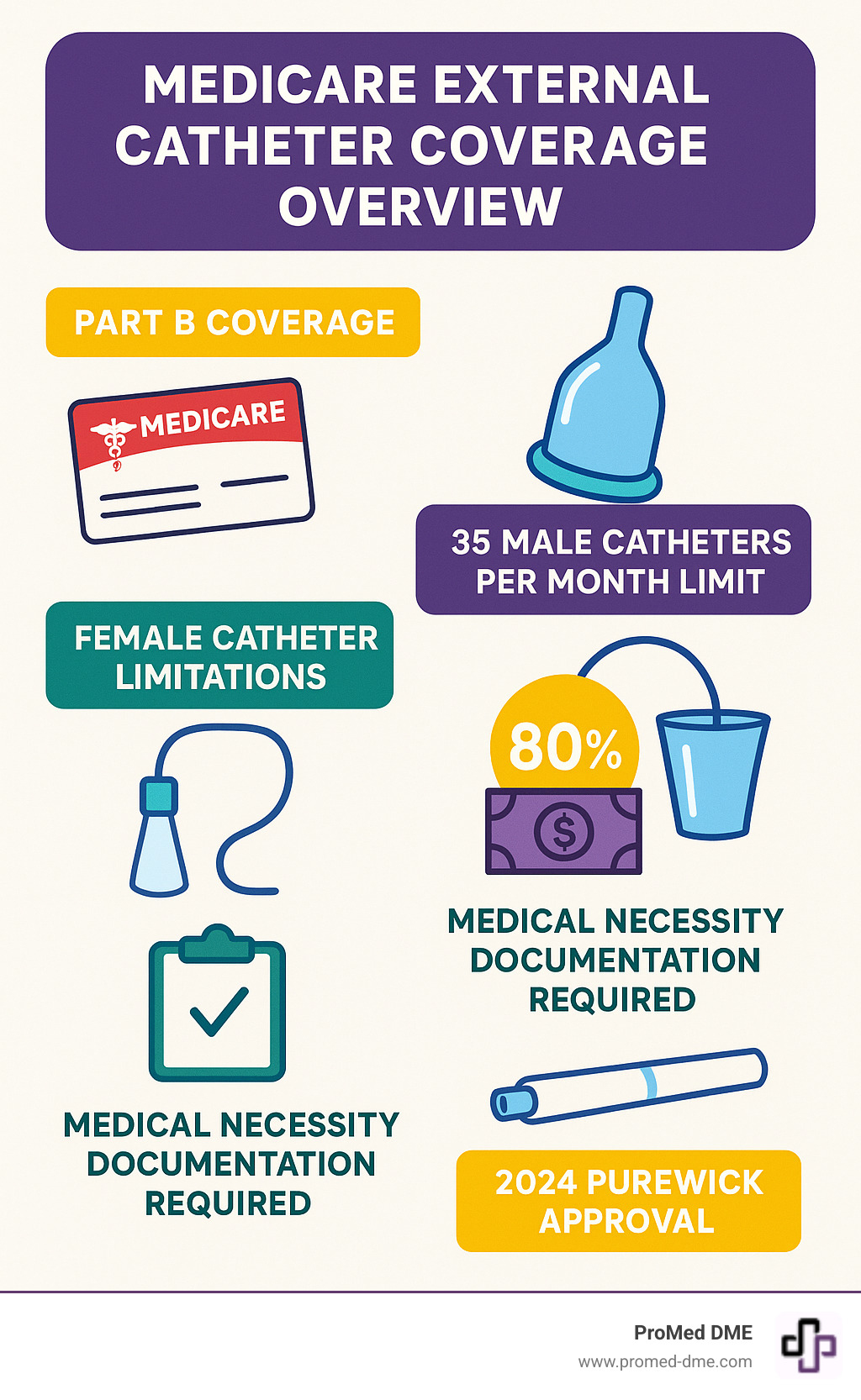
Medicare does cover external catheters when they're deemed medically necessary. Here's a quick overview of what's covered:
| Coverage Point | Details |
|---|---|
| Medicare Part | Part B (as Durable Medical Equipment) |
| Male Catheters | Up to 35 per month |
| Female Catheters | One pouch per day or one metal cup per week |
| Cost Share | 80% covered after meeting $257 deductible (2025) |
| Requirements | Permanent incontinence expected to last 3+ months |
| 2024 Update | PureWick Female External Catheter System now covered |
For many people managing urinary incontinence, external catheters provide a vital non-invasive alternative to indwelling catheters. These devices - which include condom-style catheters for men and collection systems like PureWick for women - help maintain dignity and independence while reducing complications associated with internal catheterization.
Managing incontinence is challenging enough without worrying about insurance coverage. Whether you're exploring options for yourself or a loved one, understanding exactly what Medicare covers can save you significant out-of-pocket expenses and help you access the supplies you need.
This comprehensive guide will walk you through everything you need to know about Medicare coverage for external catheters - from eligibility requirements and documentation needs to quantity limits and recent coverage updates.
Why This Guide Matters
There's a significant information gap when it comes to understanding Medicare coverage for specialized medical supplies like external catheters. Many beneficiaries and caregivers struggle to steer the complex rules and documentation requirements, often resulting in unexpected expenses or denied claims.
Cost concerns are legitimate – without insurance coverage, a box of 30 female external catheters can cost approximately $209 out of pocket. For those on fixed incomes, these expenses can be prohibitive without proper Medicare coverage.
Medicare's rules regarding external catheters can be confusing, with different coverage criteria for male versus female devices, varying quantity limitations, and specific documentation requirements that must be met. Our goal is to explain these rules so you can access the supplies you need with minimal hassle.
Who Should Read
This guide is designed for:
- Medicare beneficiaries who need external catheters for managing urinary incontinence
- Caregivers and family members helping loved ones steer Medicare coverage
- Healthcare professionals seeking to help patients obtain necessary supplies
- Anyone transitioning from hospital to home care who needs to understand how coverage changes
Understanding External Catheters
Before diving into Medicare coverage details, let's clarify what external catheters are and how they work.
External catheters are non-invasive urinary collection devices that, unlike indwelling catheters, don't require insertion into the urethra. They sit outside the body, collecting urine and directing it to a collection bag or container – providing a more comfortable and less invasive solution for many people managing incontinence.
How External Catheters Work
Think of external catheters as a gentle "catch and channel" system rather than the "plug and drain" approach of internal catheters. They work through non-invasive urine diversion – creating a pathway for urine to flow away from the body without any uncomfortable insertion.
For men, a soft, flexible condom-style sheath rolls over the penis and connects to drainage tubing. The urine flows naturally into this sheath and down into a collection bag that can be discreetly attached to the leg or hung beside the bed.
For women, systems like PureWick use a different approach. A soft, absorbent wick is placed between the legs, where it gently draws urine away through mild suction from a small, quiet pump. The collected urine moves to a container that sits beside the bed – no internal devices needed!
Male vs. Female Designs
Men and women have different anatomical needs when it comes to external catheters, and Medicare covers different types and quantities for each.
Men typically use condom-style catheters (also called sheaths). These flexible tubes roll onto the penis like a condom and connect to drainage tubing. They come in various sizes – finding the right fit is crucial for comfort and preventing leaks. Medicare will cover up to 35 of these per month for qualifying beneficiaries.
Women have several external options, including adhesive collection pouches that attach to the perineal area, meatal cups that fit over the urethral opening, and wicking systems like PureWick. Under standard Medicare guidelines, women can receive one collection pouch per day or one metal cup per week.
The good news? Since 2024, Medicare now covers the PureWick Female External Catheter System – a game-changer for many women who previously had limited options.
Benefits & Potential Risks
External catheters offer several advantages that make them worth considering if you're managing incontinence.
Using external rather than internal catheters can significantly reduce UTI risk – a common and serious complication with indwelling catheters. They're also generally more comfortable since there's no insertion involved, which helps preserve dignity and independence.
Many users find they can apply their external catheters themselves, increasing their self-sufficiency. When used correctly, these devices help maintain skin integrity by keeping moisture away from sensitive areas.
Of course, nothing is perfect. External catheters do require attention to prevent issues:
Skin irritation can develop if the catheter isn't changed regularly – most healthcare providers recommend changing every 24-48 hours. Some users experience allergic reactions to latex or adhesive materials (silicone options are available for those with sensitivities).
Proper sizing is essential – too loose and you'll experience leakage, too tight and you'll have discomfort. It may take some trial and error to find your perfect fit.
"External catheters offer a non-invasive solution that reduces discomfort and UTI risk compared to indwelling catheters," notes a urological supply specialist. "However, proper sizing, application, and regular changes are essential to prevent complications."

Does Medicare Cover External Catheters?
Yes, Medicare does cover external catheters when they're medically necessary for your condition. This coverage falls under Medicare Part B as durable medical equipment (DME) and is specifically classified under the Prosthetic Device benefit according to Social Security Act §1861(s)(8).
To qualify, you need to have permanent urinary incontinence or retention that your doctor expects will last at least three months. Don't worry—"permanent" doesn't mean you'll never improve. It simply means your condition is expected to continue beyond that three-month threshold, as determined by your healthcare provider.
For all the nitty-gritty details on coverage criteria, you can check out the Medicare Coverage Determination document. It spells out exactly what's required for Medicare to cover external catheters.
Eligibility Requirements
Getting Medicare to cover your external catheters isn't complicated, but there are a few boxes you'll need to check:
First, medical necessity is key. Your doctor must document that you have permanent urinary incontinence or retention expected to last at least three months. This documentation is crucial—without it, Medicare won't approve coverage.
You'll also need a face-to-face examination with a qualified healthcare provider. This could be your doctor, a physician assistant, nurse practitioner, or clinical nurse specialist. This requirement comes from Medicare's Final Rule 1713 and helps ensure you're getting the right supplies for your specific needs.
Before you can receive your catheters, your healthcare provider must provide a Written Order Prior to Delivery (WOPD). Think of this as your catheter prescription. It needs to include your name, the specific items ordered, your provider's NPI number, their signature, and the date.
One thing to note: Medicare won't approve external catheters if you're already using an indwelling catheter, since they serve the same purpose. It's one or the other, not both.
Quantity & Frequency Limits
Medicare has set some reasonable limits on how many external catheters you can receive:
For men, Medicare covers up to 35 male external (condom) catheters per month. That's typically enough for at least one change per day, with a few extras. If your condition requires more frequent changes, your doctor can document this need to potentially get additional coverage.
For women, coverage includes one female urinary collection pouch per day (about 30 per month) OR one metal cup per week. The recently approved PureWick system follows similar guidelines.
Here's a quick breakdown of what you can expect:
| External Catheter Type | Medicare Monthly Allowance | Notes |
|---|---|---|
| Male Condom Catheter | 35 units | More with documented need |
| Female Collection Pouch | 30 units (1 per day) | Cannot be combined with other types |
| Female Metal Cup | 4 units (1 per week) | Cannot be combined with other types |
| PureWick System | Similar to standard female limits | Newly approved in 2024 |
These limits reflect what Medicare considers "reasonable and necessary" for most people. Your healthcare provider is your best advocate if you need more.
What's Included
When Medicare covers external catheters, you're getting more than just the catheter itself. Coverage typically includes:
The external catheter (whether it's a condom catheter, female pouch, or other type), any drainage bags you need (leg or bedside), all necessary tubing and connectors, and the adhesive strips or other devices needed to secure everything in place.
It's worth noting that adhesive strips or tape used with male external catheters are included in the catheter allowance and aren't separately billable. When suppliers bill Medicare, they must use the AU modifier for certain codes when these supplies are used with urological equipment.
Not everything makes the cut, though. Medicare typically doesn't cover skin creams or barriers (unless specifically medically necessary), underpads or bed protectors, disposable incontinence garments like diapers or pull-ups, or catheter care kits not related to drainage.
Recent 2024 Updates
Great news for women with urinary incontinence! In 2024, Medicare approved the PureWick Female External Catheter System for coverage under Part B as durable medical equipment for home use.
This is a big step forward in coverage equity. Historically, women have had fewer external catheter options covered by Medicare compared to men. According to the 2024 ruling on PureWick, the system is now covered when prescribed by a Medicare-enrolled provider for beneficiaries with permanent urinary incontinence.
This expanded coverage acknowledges women's unique needs and provides a non-invasive alternative that can help reduce complications like urinary tract infections that are often associated with indwelling catheters.
At ProMed DME, we stay on top of these Medicare coverage updates so we can help you access the supplies you need with minimal hassle and expense.
Out-of-Pocket Costs & Plan Variations
Understanding what you'll actually pay for external catheters with Medicare can save you from unexpected bills and help you budget effectively.

Here's the bottom line: with Original Medicare (Part B), you'll pay the annual deductible ($257 in 2025) first, and then Medicare covers 80% of the approved amount for your external catheters and supplies. You're responsible for the remaining 20%.
Let's put that in real terms. If Medicare approves $100 for your monthly catheter supplies, you'd pay $20 out-of-pocket (after meeting your deductible). This 80/20 split applies to all durable medical equipment under Part B, including your external catheters.
If you're in the hospital, good news - external catheters used during your stay fall under Medicare Part A as part of your inpatient benefits. You'll just need to meet the Part A deductible ($1,676 in 2025).
Original Medicare vs. Medicare Advantage
The way you pay for external catheters can look quite different depending on whether you have Original Medicare or a Medicare Advantage plan.
With Original Medicare, the rules are straightforward:- You can use any Medicare-enrolled supplier nationwide- You pay 20% of the Medicare-approved amount- You generally don't need prior authorization- Your coverage is the same no matter where you live
With Medicare Advantage plans, things get more personalized:- You might pay a set copay instead of 20% coinsurance- You'll likely need to use in-network suppliers- Your plan may require prior authorization before covering supplies- Some plans offer extra benefits beyond what Original Medicare provides
"Many of our customers find that Medicare Advantage plans offer good value, but they're sometimes surprised by network restrictions," notes a customer service specialist at ProMed DME. "We always recommend checking your plan details before ordering supplies."
If you have a Medicare Advantage plan, take a few minutes to call your plan or check your benefits booklet. Medicare Advantage plans must cover at least what Original Medicare does, but the rules and costs can vary significantly.
Sample Cost Scenarios
Let's look at some real-world examples to see what you might actually pay:
For a man using external catheters with Original Medicare:After meeting your $257 annual deductible, a monthly supply of 35 catheters with a Medicare-approved amount of $140 would cost you about $28 out-of-pocket (20% of $140). Over a year, that's approximately $336 plus your deductible.
For a woman using the PureWick system with Original Medicare:A box of 30 PureWick catheters might retail for around $209, but if the Medicare-approved amount is $170, you'd pay about $34 per month (20% of $170) after meeting your deductible.
If you have a Medicare Supplement (Medigap) policy:Using the same example as above, after meeting your Part B deductible, Medicare would pay $112 (80%), your Medigap policy would cover the remaining $28 (20%), and your cost would be $0. This is why many people who use regular medical supplies choose to add a Medigap policy.
Many of our customers at ProMed DME find that having a Medicare Supplement plan provides peace of mind and predictability when budgeting for ongoing catheter supplies. We're always happy to help explain how your specific coverage works and find ways to minimize your out-of-pocket costs.
Medicare cover external catheter supplies differently depending on your plan type, so it's worth taking time to understand your specific coverage before ordering.
Step-by-Step: Getting External Catheters Through Medicare
Getting external catheters through Medicare doesn't have to be complicated. With a clear roadmap, you can steer the process smoothly and ensure you receive the supplies you need without unnecessary delays or complications.

Gather Required Documents
The first step is having a heart-to-heart with your healthcare provider about your urinary challenges. Your doctor understands both your medical needs and Medicare's requirements, making them your best ally in this process.
You'll need a Standard Written Order (SWO) from your doctor – think of this as your "prescription" for external catheters. This document needs to include your personal details, the specific type of catheter you need, how many you'll use, and how long you'll need them. The order must clearly indicate that your condition is permanent and expected to last at least three months.
Your medical records play a crucial role too. They should clearly document your diagnosis and explain why external catheters are necessary for your situation. The good news? Once Medicare establishes your initial need for these supplies, they assume ongoing need without requiring constant proof. This means less paperwork for you in the long run!
"The initial documentation is the most important," explains a Medicare specialist. "After that, Medicare understands that permanent conditions don't need to be repeatedly proven."
Choose an Approved Supplier
Finding the right supplier makes all the difference in your experience. Medicare's Supplier Directory on Medicare.gov can help you locate suppliers in your area who are enrolled in the Medicare program.
Always verify that your chosen supplier accepts "Medicare assignment" – this means they've agreed to accept Medicare's approved payment amount and can't charge you more than your 20% coinsurance (after your deductible). At ProMed DME, we not only accept Medicare assignment but serve beneficiaries nationwide with specialized urological supplies.
When contacting potential suppliers, be specific about your needs. Discuss any material preferences or allergies – for example, if you need latex-free catheters due to sensitivities. A good supplier will take time to understand your unique situation and recommend appropriate products.
Don't forget to ask about their reordering process! Understanding how far in advance you need to place orders can help prevent stressful gaps in your supply.
Submit & Track Your Claim
Once you've selected a supplier, they'll handle most of the claim submission process for you. They'll use specific HCPCS codes to identify your supplies – A4349 for male external catheters or A4328 for female external catheters, along with codes for any drainage bags or accessories you need.
Your supplier will also include important modifiers with your claim, such as the KX modifier (which indicates medical necessity requirements are met) or the AU modifier for certain accessories. These little codes make a big difference in how Medicare processes your claim!
Medicare has specific rules about delivery timing to prevent waste. Your supplier can't contact you about refills until you're within 30 days of running out, and they shouldn't deliver new supplies more than 10 days before you need them. This system helps ensure you always have what you need without accumulating excess supplies.
"We understand how important timely delivery is," shares a ProMed DME representative. "That's why we process orders quickly – those placed before 1 PM typically arrive the very next business day."
What to Do if Denied
If Medicare denies coverage for your external catheters, don't panic – you have options!
Your first step is requesting a redetermination, which is Medicare-speak for "first level appeal." You'll need to submit this within 120 days of receiving your Medicare Summary Notice. Include a detailed letter from your doctor explaining why these supplies are medically necessary for your condition.
If your redetermination is unsuccessful, you can request reconsideration within 180 days. This second-level appeal goes to a different reviewer who will take a fresh look at your case. Consider including any new evidence that supports your need.
For particularly challenging cases, you can continue the appeals process through an Administrative Law Judge hearing, Medicare Appeals Council review, and even judicial review in federal court if necessary.
At ProMed DME, we understand how frustrating denials can be, especially when you're dealing with a sensitive medical condition. Our experienced team can help guide you through the appeals process, ensuring you have the best possible chance of securing the coverage you're entitled to receive.
Persistence often pays off when it comes to Medicare appeals. Many initially denied claims are approved upon review when properly documented.
Safe Use, Maintenance & Troubleshooting
Taking proper care of external catheters isn't just about comfort—it's essential for preventing complications and maintaining your health. Let's talk about how to use these devices safely in your daily life.
Think of your external catheter as something that needs regular attention—much like brushing your teeth. Change your catheter every 24-48 hours to keep your skin healthy and prevent infection. Before applying a new one, take time to thoroughly clean the area with mild soap and water. Pat dry completely, as moisture can lead to skin problems.
"I always tell my patients to make catheter changes part of their regular routine," says a urological care specialist. "And don't forget to drink plenty of water! Good hydration is one of the best ways to prevent urinary tract infections."
Make a habit of checking the skin around your catheter daily. Look for any redness, irritation, or breakdown—catching these issues early can prevent more serious problems. And remember to empty drainage bags when they're about two-thirds full. A too-full bag can pull on the catheter and cause leaks or discomfort.
Allergies & Material Selection
If you've ever had an allergic reaction to a bandage, you'll understand why material selection matters for external catheters.
Latex allergies are surprisingly common, affecting about 1-6% of the general population. If you experience itching, redness, or discomfort with latex catheters, switch to silicone or other latex-free options. The good news? Medicare will cover these alternatives when they're medically necessary.
Adhesive sensitivities can also make catheter use uncomfortable. If traditional adhesives irritate your skin, ask about silicone-based or hydrocolloid options, which tend to be gentler. Some catheters come with built-in adhesive, while others use straps instead, avoiding adhesives entirely.
"Most of our customers with sensitive skin do really well with silicone catheters," notes a ProMed DME specialist. "And don't be shy about mentioning your allergies—we've heard it all before and can help find the right product for your specific needs."
Combining with Other Devices
External catheters don't have to work alone! They can team up with other products to make your life easier.
Many people use leg bags during the day for greater mobility—these smaller drainage bags strap discreetly to your leg under clothing. Then they switch to larger bedside drainage bags at night for uninterrupted sleep. Medicare typically covers both types when prescribed alongside your external catheters.
For women using systems like PureWick, the required suction devices are also covered when medically necessary. However, it's worth noting that Medicare won't cover both indwelling and external catheters simultaneously—they're considered duplicate devices serving the same purpose.
While protective bed pads can provide peace of mind, these usually aren't covered by Medicare and would be an out-of-pocket expense. Many of our customers at ProMed DME find them worthwhile for added security, especially when first adjusting to external catheter use.
Common Complications & Solutions
Even with careful use, you might encounter some challenges with external catheters. Here's how to tackle the most common issues:
Leakage is perhaps the most frustrating problem. If you're experiencing leaks, first check your catheter size—too large or too small can both cause problems. For men using condom catheters, the sheath should fit snugly but not tightly. For women, ensure the collection device is properly positioned. Sometimes switching adhesive types or application techniques solves the problem completely.
Skin irritation often results from moisture trapped against the skin or changing catheters too infrequently. If you notice redness or discomfort, try changing your catheter more often and consider using a protective skin barrier. These thin films or creams create a protective layer between your skin and the catheter adhesive.
"One customer was changing his catheter just once every three days and developed significant irritation," shares a ProMed DME nurse. "When he switched to daily changes, the problem resolved within a week."
Dislodgement typically happens during sleep or physical activity. Secure straps can help keep everything in place, especially for more active users. Some people find that applying the catheter after a warm shower, when skin is clean and dry, improves adhesion significantly.
If you develop symptoms of a urinary tract infection—burning, frequency, cloudy urine, or fever—contact your healthcare provider promptly. While external catheters reduce UTI risk compared to indwelling types, infections can still occur, especially with improper hygiene or infrequent changes.
At ProMed DME, we understand that adjusting to external catheter use takes time. Our dedicated nurse is always available to help troubleshoot issues and recommend solutions custom to your specific situation. Sometimes a small adjustment makes all the difference in comfort and effectiveness.
Frequently Asked Questions about Medicare & External Catheters
We hear these questions almost every day from our customers, so you're definitely not alone if you've been wondering about these things!
Does Medicare cover external catheters for both men and women?
Yes, Medicare covers external catheters for both men and women when they're medically necessary. The coverage looks a bit different depending on your needs:
For men, Medicare typically covers the condom-style catheters that fit over the penis. For women, Medicare covers collection pouches, metal cups, and (good news!) as of 2024, the PureWick system is now covered too.
There's an important difference in the quantity limits, though. Men can receive up to 35 external catheters per month, while women are limited to one collection pouch per day or one metal cup per week. This difference reflects the different designs and intended use patterns of these devices.
How many external catheters will Medicare pay for each month?
The monthly allowance depends on which type of catheter you need:
For men, Medicare covers up to 35 external catheters per month. This typically works out to about one per day, with a few extras to account for changes needed due to leakage or other issues.
For women, coverage is limited to one collection pouch per day (about 30 per month) or one metal cup per week (about 4 per month).
If your medical situation requires more than these standard amounts, don't worry! Your healthcare provider can document your medical necessity for additional quantities, and Medicare may approve the higher amount.
What happens if my doctor says my condition isn't permanent yet?
This is where things can get a bit tricky. Medicare requires that your urinary incontinence or retention be "permanent," which they define as a condition expected to last at least 3 months.
If your doctor believes your condition is temporary or will resolve within 3 months, Medicare typically won't cover external catheters during that period. You'd need to use other payment options until you meet that threshold.
However—and this is important—if your doctor anticipates your condition will last beyond 3 months, you may still qualify for coverage even if some improvement is possible. "Permanent" in Medicare-speak doesn't necessarily mean "forever"—it just means "long-term enough" to qualify.
Can I use external catheters if I have an indwelling catheter?
No, Medicare won't cover both at the same time. Medicare considers external and indwelling catheters to be duplicate devices serving the same purpose. You'll need to choose which type works best for your situation based on your medical needs and personal preferences.
Your doctor can help you decide which option is right for you, considering factors like comfort, infection risk, and ease of use.
What documentation do I need to get Medicare to cover my external catheters?
To get Medicare cover external catheter supplies, you'll need:
A Standard Written Order from your healthcare provider that includes:- Your personal information- The specific type and quantity of catheters needed- Duration of need (indicating the condition is expected to last 3+ months)- Relevant diagnosis codes (ICD-10)- Your provider's signature and NPI number
Your medical records should also clearly document your urinary condition and explain why external catheters are necessary for managing it. At ProMed DME, we can help guide you through this paperwork process—we've helped thousands of patients successfully steer these requirements.
How do I know what size or brand of external catheter is right for me?
Finding the right fit is crucial for both comfort and function. Your healthcare provider should help determine the appropriate size and brand based on your anatomy and specific needs.
For men, external catheters are typically measured in millimeters or French sizes, indicating the diameter. Getting the right fit is a bit like Goldilocks—too tight can cause discomfort and restriction of blood flow, while too loose can lead to embarrassing leakage.
At ProMed DME, our dedicated nurse can help guide you through sizing questions if you're unsure. Many of our customers find that trying a sample pack with different sizes helps them find their perfect fit.
What if I have allergies to latex or adhesives?
Allergies are very common and nothing to worry about! If you have latex allergies, silicone or other latex-free catheter options are readily available and covered by Medicare when medically necessary.
For those with sensitive skin or adhesive allergies, several alternatives exist:- Silicone-based adhesives (often gentler on skin)- Hydrocolloid options (can be better for sensitive skin)- Self-adhering catheters that don't require separate adhesive- Strap-secured catheters that avoid adhesives entirely
Be sure to mention any allergies or sensitivities to both your healthcare provider and your medical supplier. At ProMed DME, we keep detailed notes on customer allergies to ensure you never receive products that could cause a reaction.
How often should I change my external catheter?
For best results and to prevent complications, external catheters should typically be changed every 24-48 hours. This regular changing helps maintain skin integrity and prevents infection.
Some patients find they need to change more frequently based on their activity level, perspiration, or other factors. Follow your healthcare provider's recommendations and the manufacturer's guidelines for your specific catheter type.
Medicare's monthly allowances are designed with these recommended changing intervals in mind, which is why they provide approximately 30-35 devices per month for daily use.
Conclusion
Navigating Medicare coverage for external catheters doesn't have to feel like solving a puzzle. With the right information in hand, you can access the supplies you need while keeping your out-of-pocket costs manageable.
Let's recap what we've learned about Medicare coverage for external catheters:
- Medicare Part B covers these devices when prescribed for permanent urinary incontinence or retention that's expected to last at least three months
- For men, Medicare allows up to 35 external catheters monthly – enough for daily changes with some extras
- Women can receive one collection pouch daily or one metal cup weekly, with similar guidelines for the newly-covered PureWick system
- After meeting your annual deductible, Medicare handles 80% of the approved amount, leaving you responsible for the remaining 20%
- Your healthcare provider's detailed documentation is absolutely essential for securing coverage
- The 2024 approval of the PureWick system represents a significant step forward in coverage options for women
At ProMed DME, we understand that managing urinary incontinence presents enough challenges without adding insurance headaches to the mix. That's why we've designed our service to make the entire process simpler and more dignified for you.
Our team offers several advantages that our customers appreciate:
Free shipping means no extra costs for delivery, regardless of where you live in the United States. Our dedicated nurse on staff is available to answer your questions about product selection, usage, and troubleshooting – bringing professional healthcare guidance right to your home. With nationwide delivery from our Stuart, Florida headquarters, we serve Medicare beneficiaries across the country.
We also handle the paperwork burden by providing assistance with insurance verification and claims processing. And our automatic refill reminder system ensures you'll never face the stress of running out of essential supplies.
Living with urinary incontinence shouldn't mean sacrificing your independence or dignity. The right external catheter, properly covered by Medicare, can help maintain your quality of life and prevent complications that might arise from other management methods.
For more information about our external catheter supplies and Medicare billing services, visit ProMed DME's website or call our friendly customer service team. We're committed to providing top-quality urological supplies with genuine care and understanding to Medicare beneficiaries nationwide.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.




