Why Your Blood Sugar Takes a Dive: A Guide to Hypoglycemia Causes
Understanding What Makes Your Blood Sugar Drop
What causes hypoglycemia can be broken down into several key factors that affect people with and without diabetes:
For People With Diabetes:
- Taking too much insulin or diabetes medication
- Not eating enough carbohydrates for the insulin taken
- Skipping or delaying meals
- Increased physical activity without adjusting medication
- Drinking alcohol, especially on an empty stomach
For People Without Diabetes:
- Certain medications (beta-blockers, antibiotics)
- Critical illnesses affecting liver or kidney function
- Hormone deficiencies
- Excessive alcohol consumption
- Eating disorders like anorexia nervosa
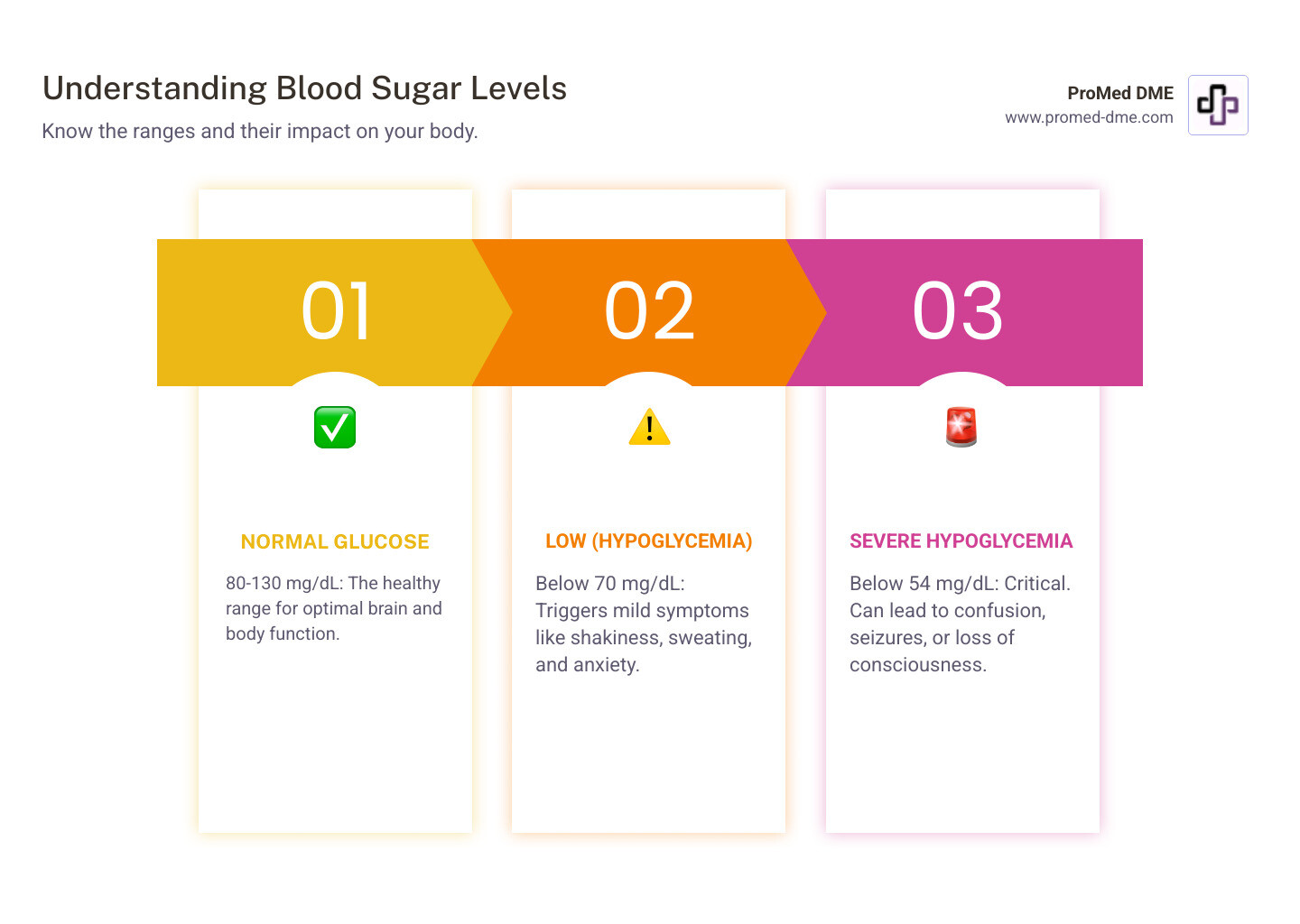
Hypoglycemia, or low blood sugar, happens when your blood glucose drops below 70 mg/dL. Your brain depends on a steady supply of glucose to function properly - it can't store or make its own energy like other organs can.
This condition affects millions of Americans. Research shows that 4 out of 5 people with type 1 diabetes experience at least one low blood sugar episode every month. Even people with type 2 diabetes who take insulin face this challenge regularly.
The symptoms can range from mild shakiness and sweating to severe confusion, seizures, or loss of consciousness. Without quick treatment, hypoglycemia can become life-threatening.
Understanding the root causes helps you prevent dangerous episodes and manage your blood sugar more effectively. Whether you have diabetes or not, knowing these triggers can help you stay safe and healthy.
Know your what causes hypoglycemia terms:
Understanding Hypoglycemia: Symptoms and Levels
When we explore what causes hypoglycemia, first recognize how low blood sugar feels and understand the danger zones. Your body is remarkably good at sending warning signals when glucose levels start dropping - you just need to know what to listen for.
Hypoglycemia kicks in when your blood glucose falls below 70 mg/dL if you have diabetes. For people without diabetes, the threshold is typically around 55 mg/dL. But here's what really matters: severe hypoglycemia begins at 54 mg/dL, and that's when things get serious fast.

Think of your body's early warning system like a car's dashboard lights. When that fuel gauge starts blinking, you don't ignore it - and you shouldn't ignore these symptoms either.
Recognizing Early Warning Signs
Your body doesn't give up without a fight when blood sugar drops. Those first symptoms are actually your body's way of screaming "Hey, I need fuel!"
Shaking and sweating are often the first things you'll notice. Your hands might tremble, and you could break out in a cold sweat even when you're perfectly comfortable temperature-wise. Your heart starts racing like you just ran up a flight of stairs, and you might feel anxious or irritable for no obvious reason.
Hunger hits hard and fast - not the gentle "I should probably eat soon" feeling, but an urgent, almost desperate need for food. You might also notice your skin looks pale, and dizziness or lightheadedness can make you feel unsteady on your feet.
These mild symptoms typically show up when your blood glucose hovers around 70 mg/dL. The good news? Acting quickly on these early signs by eating or drinking something with fast-acting carbs can stop the episode in its tracks.
Symptoms of Severe Hypoglycemia
When blood sugar continues dropping below 54 mg/dL, your brain - which depends entirely on glucose for fuel - starts struggling to function properly. This is where hypoglycemia becomes genuinely dangerous.
Vision problems are common - things might look blurry or you might see double. Your speech becomes slurred, making it hard to communicate clearly. Clumsiness and poor coordination can make simple tasks like walking or picking up objects nearly impossible.
Confusion and disorientation set in, leaving you feeling lost even in familiar places. Some people experience severe headaches, while others feel overwhelmingly weak and fatigued.
In the most serious cases, seizures can occur, or you might lose consciousness entirely. These are medical emergencies that require immediate help - no exceptions.
Understanding these warning signs isn't just important for you - it's crucial for your family members and close friends too. They need to recognize when you're in trouble and know how to respond. For comprehensive information about managing these episodes, check out Low Blood Glucose (Hypoglycemia) from NIDDK.
The key is catching these symptoms early and taking action fast. Your body is trying to protect you - listen to what it's telling you.
What Causes Hypoglycemia in People with Diabetes?
If you're living with diabetes, understanding what causes hypoglycemia isn't just helpful—it's essential for staying safe every day. The irony is that the very medications designed to keep your blood sugar in a healthy range can sometimes push it too low.
The main players here are insulin and certain diabetes medications like sulfonylureas (think glyburide or glipizide) and meglitinides (like repaglinide). These work by either replacing the insulin your body can't make or helping your pancreas pump out more of its own insulin. It's like having a helpful assistant that sometimes gets a little too enthusiastic about the job.
Whether you have type 1 diabetes (where your pancreas has basically gone on permanent vacation from insulin production) or type 2 diabetes (where your body either doesn't make enough insulin or doesn't use it well), managing your blood sugar is like walking a tightrope. You're constantly balancing medication, food, and activity—and sometimes life throws you a curveball.
Common triggers: what causes hypoglycemia from day to day?
Let's get real about the everyday situations that can send your blood sugar tumbling. Too much insulin or diabetes medication is the biggest culprit. Maybe you accidentally gave yourself rapid-acting insulin instead of your long-acting dose, or perhaps you forgot you already took your medication and doubled up. We've all had those moments where our brain feels like it's running on empty.
Medication timing can be tricky too. Taking your insulin and then getting distracted by a phone call, only to realize an hour later that you never ate—that's a recipe for trouble. Your medication doesn't know you got sidetracked; it's doing its job regardless.
Skipped meals or not eating enough carbohydrates for the insulin you've taken is another common scenario. Life gets busy, meetings run long, or sometimes you're just not feeling hungry. But your medication is still working based on what you planned to eat.
Physical activity is fantastic for your health, but it makes your muscles gobble up glucose like they haven't eaten in days. If you decide to take an impromptu walk or your workout is more intense than usual, your blood sugar might drop during exercise or even hours later while you're sleeping.
Alcohol consumption deserves special mention because it's sneaky. A glass of wine with dinner might seem harmless, but alcohol interferes with your liver's ability to release stored glucose. This effect can show up hours later, sometimes causing unexpected nighttime lows.
Even hot weather can throw you for a loop by affecting how your body processes insulin. And let's not forget about schedule changes—travel, shift work, or just a particularly hectic day can disrupt your usual routine and catch you off guard.
The Role of Diet and Exercise
Here's where things get interesting. Diet and exercise are your allies in diabetes management, but they also play starring roles in what causes hypoglycemia. Think of it as a three-way dance between your medication, your food, and your activity level.
When you exercise, your muscles become more sensitive to insulin and start using glucose more efficiently. This is wonderful for your overall health, but it means you might need to adjust your insulin doses or have a pre-exercise snack. Checking your blood sugar before, during, and after activity becomes your safety net.
Your meal composition matters more than you might think. Carbohydrates are the main event when it comes to blood sugar, but fat, protein, and fiber all influence how quickly those carbs get absorbed. A meal loaded with fiber might slow down glucose absorption, which could affect your insulin timing.
If you do find yourself dealing with low blood sugar, you'll need fast-acting carbohydrates to get back on track. Glucose tablets, fruit juice, regular soda, hard candies, or even a tablespoon of honey can do the trick. Keep these handy—your future self will thank you.
Post-exercise monitoring is crucial because your blood sugar can continue dropping for hours after you've finished your workout. It's like your muscles are still saying "thank you" long after the party's over.
The American Diabetes Association has excellent guidance on preventing these episodes: Causes and How to Prevent Hypoglycemia from the American Diabetes Association.
Hypoglycemia Causes in People Without Diabetes
Here's something that surprises many people: you don't need to have diabetes to experience low blood sugar. While it's much less common, what causes hypoglycemia in people without diabetes is often more complex and can signal underlying health issues that need medical attention.
If you're experiencing symptoms like shakiness, sweating, or confusion and you don't have diabetes, don't brush it off. Your body is trying to tell you something important. Unlike diabetes-related hypoglycemia, non-diabetic low blood sugar often points to other medical conditions that disrupt your body's natural ability to keep blood sugar stable.
Getting a proper medical evaluation is crucial here. This isn't something you want to self-diagnose or ignore, especially since the underlying causes can range from medication side effects to serious medical conditions.
For a comprehensive overview of symptoms and causes, the Mayo Clinic offers excellent resources: Hypoglycemia - Symptoms and causes from Mayo Clinic.
Reactive Hypoglycemia (After Meals)
Have you ever felt shaky or dizzy a few hours after eating a big meal, especially one loaded with sweets or refined carbs? You might have experienced reactive hypoglycemia, also called postprandial hypoglycemia.
Here's what happens: when you eat foods high in simple carbohydrates, your blood sugar shoots up quickly. Your pancreas responds by releasing a surge of insulin to bring that sugar down. But sometimes it overdoes it, releasing too much insulin and causing your blood sugar to crash below normal levels.
This type of low blood sugar is particularly common in people who've had certain stomach surgeries, especially bariatric surgery like gastric bypass. These procedures change how your digestive system processes food, causing glucose to enter your bloodstream much faster than normal. The result? Your pancreas gets confused and releases way more insulin than needed.
If you notice symptoms consistently appearing 2-4 hours after meals, especially sugary ones, this could be what you're dealing with.
Investigating what causes hypoglycemia without diabetes (Fasting)
When low blood sugar happens during fasting periods or long stretches without food, the causes become more serious and require thorough medical investigation. Your doctor will need to play detective to figure out what's going wrong with your body's natural glucose regulation.
Medications are surprisingly common culprits. Beta-blockers used for high blood pressure or heart conditions can interfere with your body's ability to raise blood sugar when needed. Certain antibiotics like sulfamethoxazole and trimethoprim can also trigger episodes. Even accidentally taking someone else's diabetes medication can cause dangerous lows in non-diabetic people.
Critical illnesses can throw your entire glucose system out of whack. When your liver is severely damaged, it can't produce or release stored glucose properly - think of it as your body's glucose warehouse being out of order. Kidney disease creates problems too, since damaged kidneys can't process insulin efficiently, leading to higher insulin levels that drive blood sugar too low.
Hormone deficiencies are another piece of the puzzle. Your body relies on several hormones to keep blood sugar stable. Adrenal insufficiency (Addison's disease) means your body doesn't produce enough cortisol, a hormone that helps raise blood sugar when needed. Growth hormone deficiency and pituitary disorders can also disrupt this delicate balance.
One of the scariest but thankfully rare causes is a pancreatic tumor called an insulinoma. This tumor essentially hijacks your pancreas, forcing it to pump out insulin constantly, which keeps driving your blood sugar dangerously low.
Anorexia nervosa and prolonged starvation deplete your body's glucose stores completely. Without adequate nutrition, your body runs out of the building blocks it needs to make new glucose, leaving you vulnerable to severe lows.
Excessive alcohol consumption is particularly dangerous because alcohol blocks your liver's ability to create new glucose. If you drink heavily without eating, especially over several hours, your blood sugar can plummet to dangerous levels.
Understanding what causes hypoglycemia without diabetes requires patience and thorough medical testing, but getting to the bottom of it is essential for your health and safety.
How to Treat and Prevent Low Blood Sugar
Understanding what causes hypoglycemia is just the beginning - knowing how to respond quickly and effectively when it happens can be life-saving. Whether you're dealing with a mild episode or a severe emergency, having a solid treatment plan gives you confidence and control over your health.
The good news is that most low blood sugar episodes can be treated at home with the right supplies and knowledge. The key is acting fast and following proven steps that healthcare professionals recommend worldwide.

Immediate Treatment: The 15-15 Rule
When your blood sugar drops below 70 mg/dL, you need to act quickly. The 15-15 Rule is your best friend here - it's simple, effective, and easy to remember even when you're feeling shaky or confused.
Here's how it works: consume 15 grams of fast-acting carbohydrates, then wait 15 minutes before checking your blood sugar again. This gives your body time to absorb the glucose and start raising your levels.
The best sources of quick-acting carbs include 4 glucose tablets (the gold standard because they're measured precisely), 4 ounces of fruit juice like orange or apple juice, or 4 ounces of regular soda - not diet! You can also use 5-6 pieces of hard candy or 1 tablespoon of honey or corn syrup.
After your 15-minute wait, recheck your blood sugar with your meter. If you're still below 70 mg/dL, repeat the process. Don't be tempted to eat more than recommended - over-treating can send you on a blood sugar roller coaster that's hard on your body.
Once your levels are back in your target range, eat a follow-up snack if your next meal is more than an hour away. Something with both carbs and protein works well - think crackers with peanut butter or a piece of cheese. This helps prevent another drop.
Managing Severe Episodes and Preventing Future Lows
Severe hypoglycemia is a different story entirely. When someone can't swallow, is unconscious, or having seizures, the 15-15 rule won't work. This is when you need emergency glucagon - a hormone that tells the liver to dump stored glucose into the bloodstream.
Glucagon kits come as injections or nasal glucagon (which is easier to use). If you're at risk for severe lows, your doctor should prescribe one. Make sure your family members know exactly where it is and how to use it. After giving glucagon, always call 911 - this is still a medical emergency.
Educating your family and close friends about hypoglycemia symptoms and treatment could save your life. Consider wearing a medical alert bracelet too - it speaks for you when you can't.
Prevention is where the real magic happens. Regular monitoring with a blood glucose meter or continuous glucose monitor gives you the power to catch lows before they become dangerous. At ProMed DME, we understand how crucial reliable monitoring equipment is for staying ahead of these episodes. More info about continuous glucose monitoring can help you explore advanced options for better blood sugar management.
Sticking to a regular meal schedule helps keep your blood sugar steady. When life gets hectic and you're tempted to skip meals, consistency is your friend. Logging your blood sugar levels along with what you eat, your medications, and activity levels helps you spot patterns in what causes hypoglycemia for you personally.
This detailed tracking becomes invaluable when working with your healthcare team to fine-tune your diabetes management plan. The more you understand your unique patterns, the better you can prevent future episodes and live with greater confidence and freedom.
Frequently Asked Questions about Hypoglycemia
After learning about what causes hypoglycemia, many people have questions about specific situations they might face. Let's tackle some of the most common concerns we hear from people managing blood sugar challenges.
What is hypoglycemia unawareness?
Hypoglycemia unawareness is one of those medical terms that sounds scarier than it needs to, but it's definitely something to take seriously. Think of it as your body's alarm system going quiet when you need it most.
Normally, when your blood sugar drops, your body sends out warning signals like shakiness, sweating, or that urgent feeling of hunger. But with hypoglycemia unawareness, these warning symptoms either become very mild or disappear completely. You might not realize your blood sugar is dangerously low until you're already experiencing severe symptoms like confusion or even loss of consciousness.
This condition often develops in people who've had diabetes for many years or who experience frequent low blood sugar episodes. Your body essentially gets used to running on lower glucose levels and stops sounding the alarm. Beta-blockers, medications commonly used for high blood pressure or heart conditions, can also mask the typical symptoms by preventing that telltale fast heartbeat.
The increased risk here is significant. Without those early warning signs, you could find yourself in a medical emergency without any heads-up. This is exactly why continuous glucose monitors can be such game-changers for people with hypoglycemia unawareness - they act as your external alarm system, alerting you to dropping blood sugar levels even when your body stays silent.
How often do people with type 1 diabetes experience low blood sugar?
The honest answer? More often than most people realize, and it's one of the daily realities of managing type 1 diabetes.
People with type 1 diabetes typically experience symptomatic low blood sugar episodes up to twice a week. But here's what's really eye-opening - a large international study found that 4 out of 5 people with type 1 diabetes reported at least one low blood sugar event over just a four-week period. Even nearly half of people with type 2 diabetes who take insulin experienced lows during that same timeframe.
These numbers aren't meant to be discouraging - they're meant to show you that if you're dealing with frequent lows, you're absolutely not alone. It's also why having reliable monitoring equipment and a solid management plan is so crucial. The importance of continuous glucose monitoring becomes crystal clear when you see how common these episodes really are.
How does alcohol affect blood sugar levels?
Alcohol and blood sugar have a complicated relationship that catches many people off guard. Understanding this connection is key to preventing alcohol-related hypoglycemia.
Here's what happens in your body: Your liver normally acts like a glucose warehouse, releasing stored sugar and creating new glucose when your blood sugar starts to drop. But when you drink alcohol, your liver gets distracted. It prioritizes breaking down the alcohol, which means it can't do its usual job of maintaining your blood sugar levels.
The tricky part is timing - alcohol's effect on blood sugar can be delayed by several hours. You might have a few drinks with dinner and feel fine, only to experience hypoglycemia later that night or even the next morning. This delayed reaction makes alcohol-related lows particularly dangerous because they often happen when you're sleeping.
Alcohol also creates a perfect storm by masking hypoglycemia symptoms. The confusion, dizziness, or slurred speech you might attribute to having a few drinks could actually be signs of low blood sugar. This makes it much harder to recognize when you need treatment.
Drinking on an empty stomach significantly increases your risk because there's less food-derived glucose to help maintain your blood sugar levels. The safest approach is to always eat when you drink, monitor your blood sugar more frequently during and after drinking, and be prepared for the possibility of delayed lows.
If you take insulin or diabetes medications, it's worth having a conversation with your healthcare provider about how to safely enjoy alcohol while minimizing your risk of dangerous blood sugar drops.
Conclusion
Now that we've explored what causes hypoglycemia together, you have the knowledge to protect yourself and your loved ones from dangerous blood sugar drops. Whether you're managing diabetes with insulin and medications, or you're experiencing unexplained low blood sugar episodes, understanding these triggers puts you in the driver's seat of your health.
Hypoglycemia isn't just about one single cause - it's about how medication timing, meal schedules, physical activity, and even unexpected life changes all work together to affect your blood sugar. For people with diabetes, it's that delicate balancing act between insulin, food, and activity. For those without diabetes, it might signal an underlying condition that needs medical attention.
The symptoms we've discussed - from the early shakiness and sweating to the more serious confusion and seizures - are your body's way of asking for help. Listen to these signals, and don't hesitate to act quickly with the 15-15 rule for mild episodes or emergency glucagon for severe ones.
But here's the thing: you don't have to manage this alone. Regular monitoring with reliable equipment makes all the difference in catching lows before they become dangerous. Having a consistent meal schedule, educating your family and friends, and keeping detailed logs of your blood sugar patterns are all powerful tools in your prevention toolkit.
At ProMed DME, we understand that managing your blood sugar is a 24/7 commitment. That's why we're here to support you with the medical supplies and monitoring equipment you need, backed by our dedicated nursing staff and commitment to working with your insurance to keep costs manageable.
Your health journey is unique, and working closely with your healthcare provider to understand what causes hypoglycemia in your specific situation is the best path forward. With the right knowledge, tools, and support system, you can live confidently while keeping those blood sugar levels right where they need to be.
Take the next step in managing your diabetes with confidence: Learn more about managing your diabetes with continuous glucose monitoring.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.




