Beyond the Abbreviation: Demystifying BPH and Your Prostate Health
Why Understanding BPH Matters for Your Health
What is BPH is a common question men ask as they age. By age 60, about 50% of men show signs of BPH, and by age 85, that number jumps to 90%.
Quick Answer: What is BPH?
- BPH stands for Benign Prostatic Hyperplasia - a non-cancerous enlargement of the prostate gland
- It's extremely common - affecting most men as they age
- It causes urinary symptoms like frequent urination, weak stream, and nighttime bathroom trips
- It's not cancer - BPH does not increase your risk of prostate cancer
- It's treatable - many options exist from lifestyle changes to medications to procedures
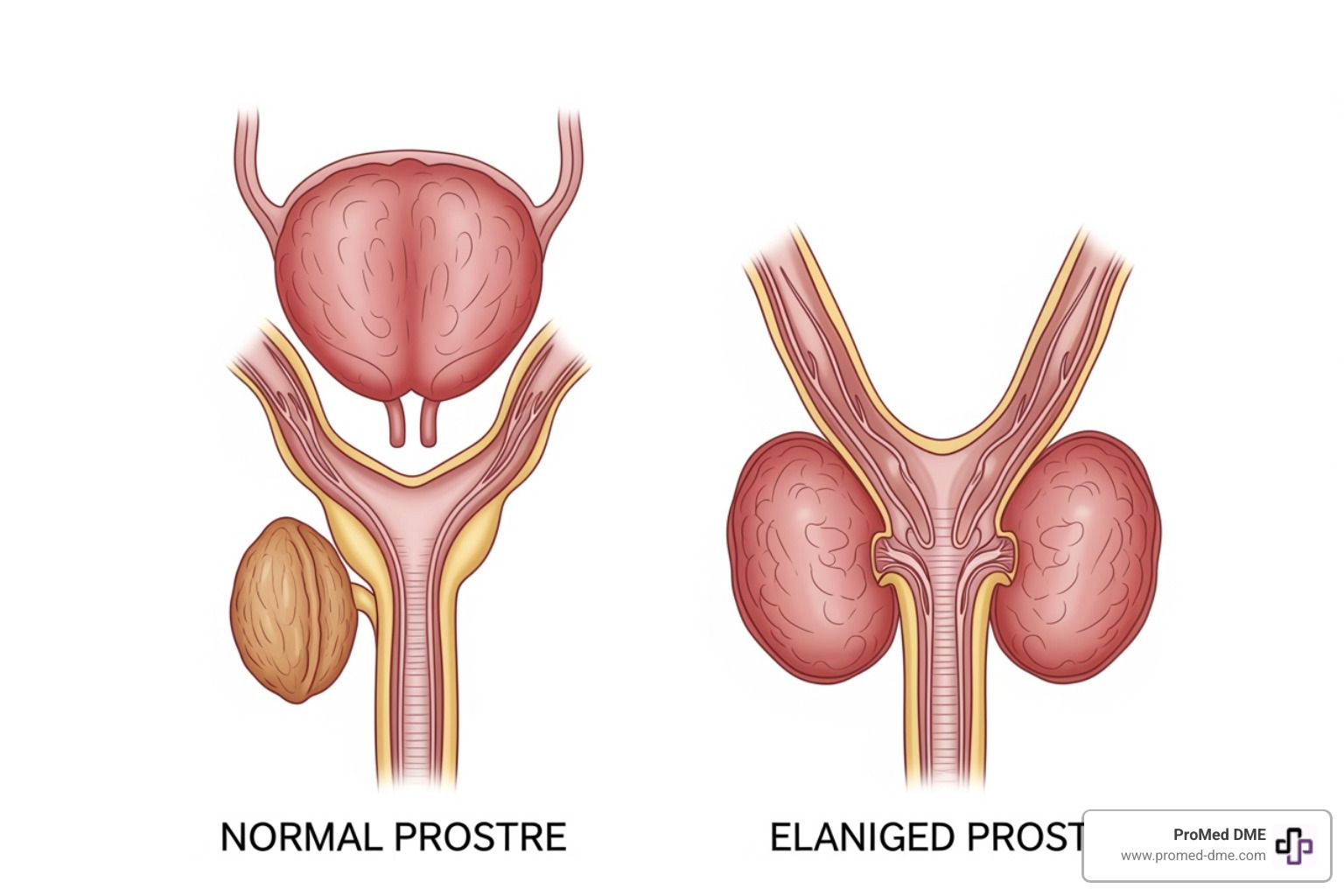
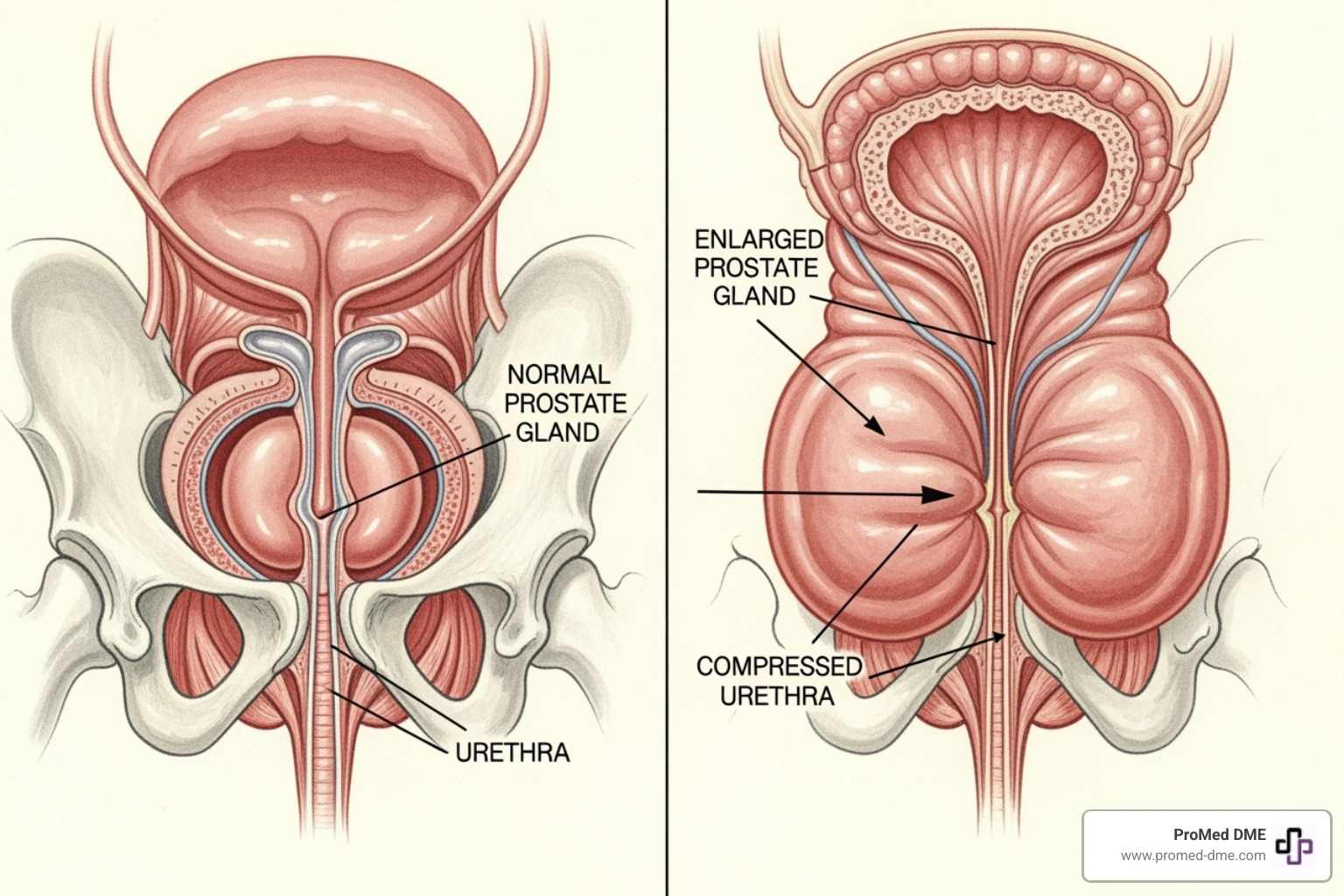
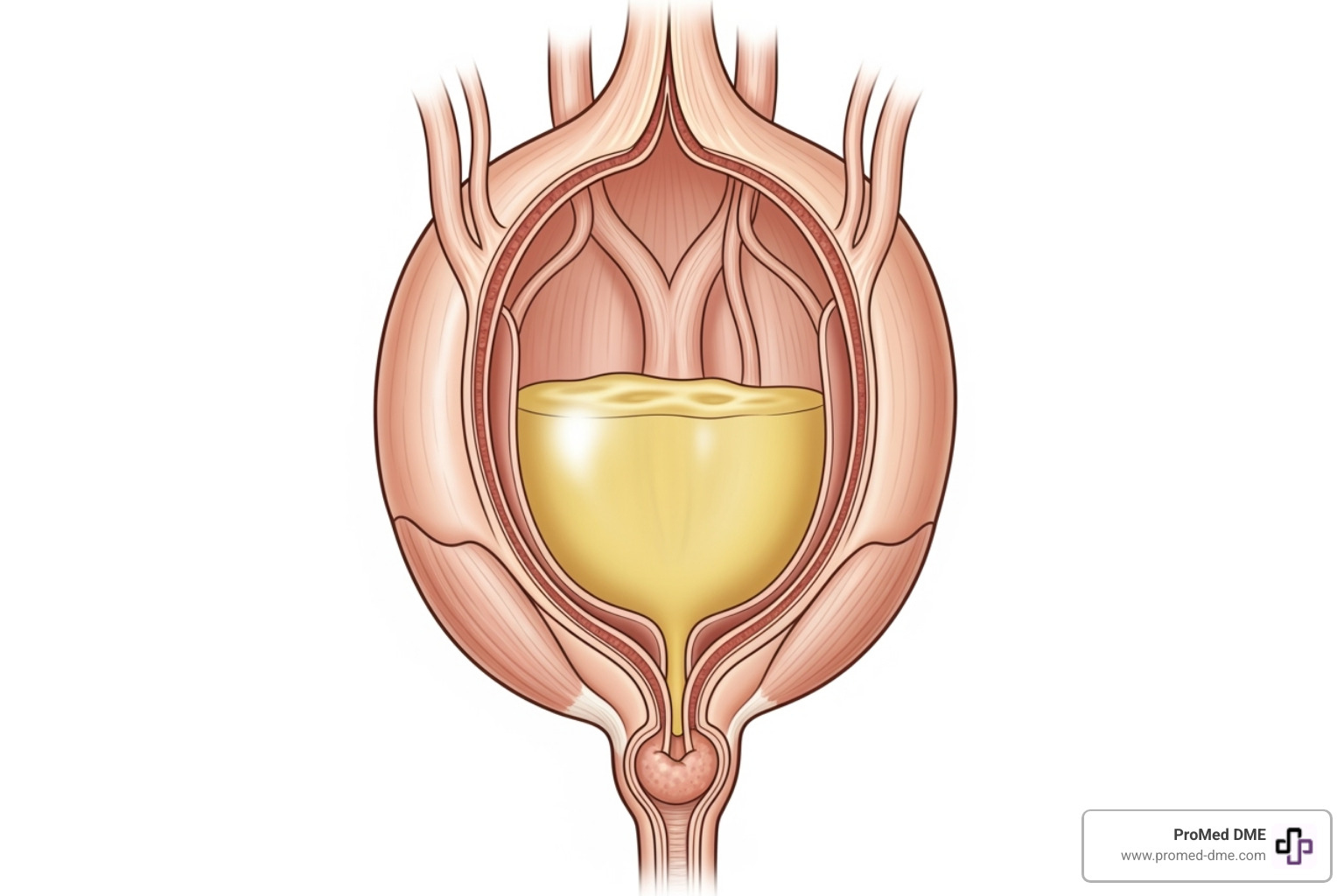
If you're constantly waking up at night to use the bathroom, you could be dealing with BPH. This condition affects the walnut-sized prostate gland located below the bladder, which surrounds the urethra—the tube that carries urine out of your body.
As your prostate grows with age, it can squeeze the urethra like a clamp on a garden hose. This pressure creates the frustrating urinary symptoms that lead many men to seek answers.
The good news is that BPH is manageable. Whether you have mild symptoms or more serious complications, solutions exist to help you regain control of your daily life.
So, What is BPH (Benign Prostatic Hyperplasia) Exactly?
What is BPH comes down to a simple, non-cancerous enlargement of the prostate gland. BPH, or Benign Prostatic Hyperplasia, is a common part of aging—inconvenient but not dangerous.
Your prostate is a walnut-sized gland below your bladder that wraps around the urethra. It produces fluid for semen. Problems arise when this gland grows larger over time.
Your prostate has two main growth phases. The first is during puberty. The second phase begins around age 25 and continues throughout life. This slow, continuous growth is what eventually leads to BPH symptoms.
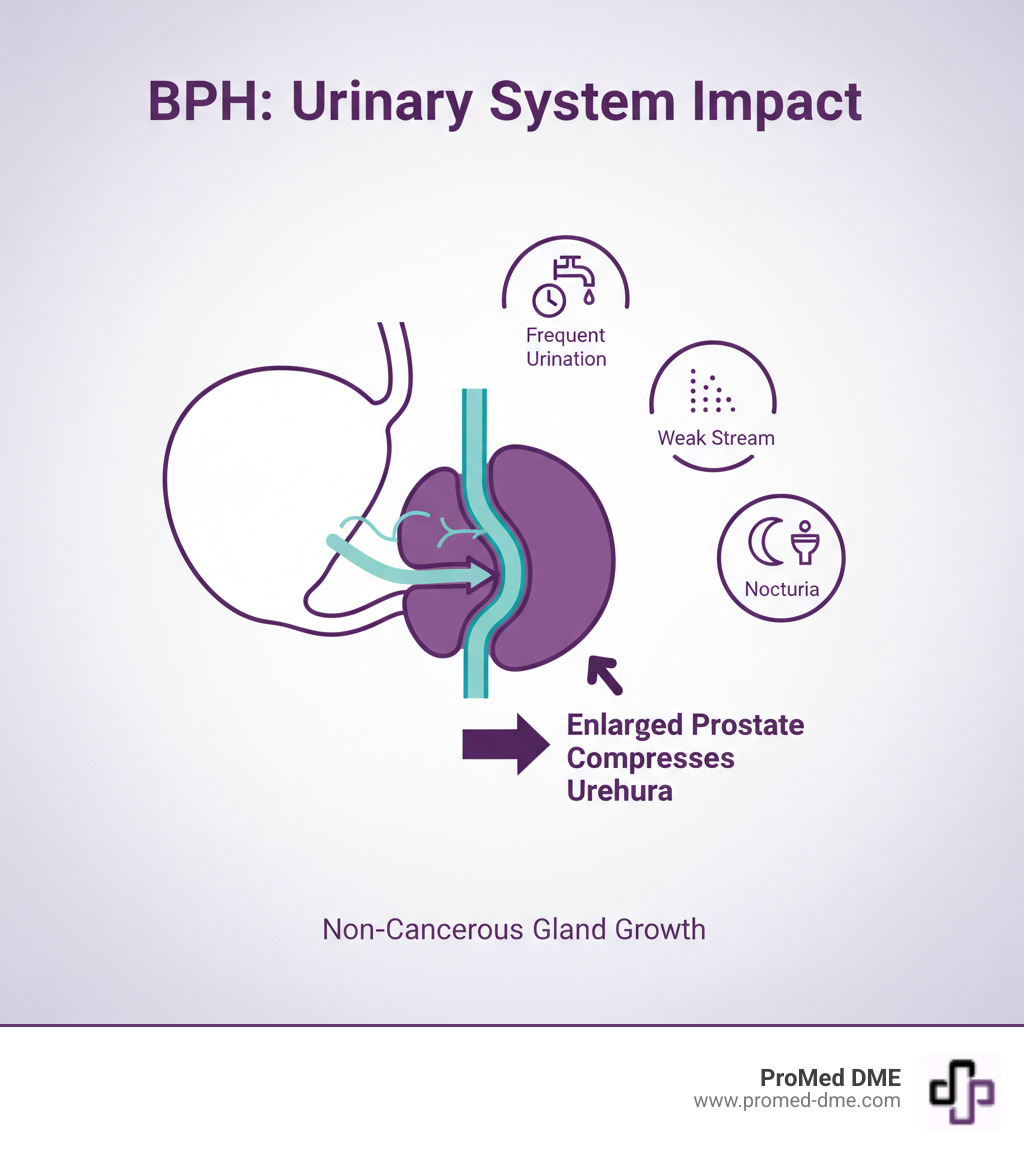
As the prostate enlarges, it presses on the urethra, obstructing urine flow. This pressure causes what doctors call Lower Urinary Tract Symptoms (LUTS), which can complicate your bathroom habits.
The key thing to remember is that this growth is benign—it won't spread to other parts of your body like cancer.
Understanding the Common Symptoms of BPH
BPH symptoms can range from mild to life-disrupting. They fall into two categories: storage symptoms (how the bladder holds urine) and voiding symptoms (how it empties).
Common storage symptoms include:
- Frequency: Needing to urinate often, sometimes every hour or two.
- Urgency: A sudden, overwhelming need to find a bathroom immediately.
- Nocturia: Waking up multiple times each night to urinate, leading to fatigue.
Common voiding symptoms include:
- Weak stream: A decreased force of urination.
- Straining: Difficulty starting or maintaining urination.
- Intermittency: The urine stream stopping and starting.
- Incomplete emptying: A feeling that the bladder isn't fully empty after urinating.
- Dribbling: Leaking urine after you think you're finished.
Prostate size doesn't always correlate with symptom severity. Some men with very large prostates have few symptoms, while others with slight enlargement struggle. About half of all men with BPH will eventually require some form of treatment.
Causes and Key Risk Factors
While the exact cause of BPH is not fully understood, several key factors are involved. The biggest risk factor is aging; BPH rarely affects men under 40, but the risk increases with each decade.
Hormonal changes are also a major contributor. Age-related shifts in hormones, including testosterone and dihydrotestosterone (DHT), encourage prostate growth.
Other key risk factors include:
- Family history: You're more likely to develop BPH if your father or brother had it.
- Obesity: Being overweight increases your risk.
- Co-existing conditions: Heart disease and Type 2 diabetes are linked to BPH.
- Lack of exercise: A sedentary lifestyle is a known risk factor. Conversely, scientific research on lifestyle changes for BPH shows that regular exercise can help reduce your risk.
While you can't change your age or genetics, managing lifestyle factors can help reduce BPH's impact.
How BPH is Diagnosed by a Healthcare Provider
To determine if BPH is the cause of your symptoms, your doctor will perform a thorough evaluation.
This process typically includes:
- Medical history: Your doctor will ask about your symptoms, possibly using a questionnaire like the International Prostate Symptom Score (IPSS) to gauge severity.
- Physical exam: This includes a Digital Rectal Exam (DRE), a quick procedure where the doctor feels the prostate's size and texture.
- Urinalysis: A urine sample is checked for infection or blood.
- PSA blood test: This measures prostate-specific antigen levels. Levels can be liftd in both BPH and prostate cancer, so your doctor will interpret the results in context.
- Uroflowmetry: You urinate into a special device that measures the speed and volume of your urine flow to check for obstruction.
- Post-void residual volume: An ultrasound is used after urination to see how much urine remains in your bladder.
Based on these findings, your doctor can confirm a BPH diagnosis and rule out other conditions.
A Guide to BPH Treatment and Management Options
Once you have a BPH diagnosis, you don't have to live with the discomfort. A range of treatment options can be custom to your specific needs.
When recommending a treatment, your healthcare provider will consider the severity of your symptoms, your prostate size, your overall health, and how BPH is affecting your quality of life. The goal is to find the most effective path to relieve your symptoms and restore comfort.

Lifestyle Adjustments and Watchful Waiting
For mild symptoms that aren't disruptive, your doctor may suggest "watchful waiting." This involves monitoring your condition with regular check-ups while making smart lifestyle changes.
- Fluid management: Limit drinks an hour or two before bedtime or before going out to reduce bathroom trips.
- Dietary changes: Cutting back on caffeine and alcohol, especially in the evening, can help since both can irritate the bladder.
- Bladder training: This involves scheduling bathroom visits to retrain your bladder to hold urine for longer.
- Double voiding: After urinating, wait a moment and try again to ensure your bladder is completely empty.
- Pelvic floor exercises: Strengthening these muscles can improve bladder control and reduce dribbling.
- Stay active: Maintaining a healthy weight and exercising regularly can help manage BPH symptoms, as obesity is a known risk factor.
- Review medications: Avoid certain over-the-counter medications like decongestants and some antihistamines, which can worsen BPH symptoms. Always inform your doctor about all medications you take.
Medications and Minimally Invasive Procedures
If lifestyle changes aren't enough, medical treatments can offer significant relief.
Medications are often the next step:
- Alpha-blockers (e.g., tamsulosin, doxazosin) relax the muscles in the prostate and bladder neck, improving urine flow. They work quickly but don't shrink the prostate.
- 5-alpha reductase inhibitors (e.g., finasteride, dutasteride) block the hormones that cause prostate growth, which can shrink the prostate over time. It may take six months or more to see full results.
- Combination therapy using both types of medication may be recommended.
- Tadalafil (Cialis), also used for erectile dysfunction, is approved to treat BPH symptoms.
Minimally invasive procedures offer a middle ground between medication and surgery:
- Water vapor thermal therapy (Rezūm) uses steam to destroy excess prostate tissue.
- Prostatic urethral lift (UroLift) uses tiny implants to hold enlarged prostate tissue away from the urethra, improving flow with fewer sexual side effects than other treatments.
Surgical Options for Severe BPH
Surgery is typically recommended for severe symptoms, when other treatments fail, or if complications like bladder stones or kidney damage develop.
- Transurethral resection of the prostate (TURP): Considered the gold standard, this procedure involves removing excess prostate tissue through the urethra. It provides significant symptom relief, though retrograde ejaculation is a common side effect.
- Laser therapy: Options like Holmium laser enucleation (HoLEP) and photoselective vaporization (PVP or GreenLight Laser) use lasers to remove or vaporize obstructing prostate tissue. These are effective for large prostates and for men on blood thinners.
- Simple prostatectomy: For extremely large prostates, this surgery involves removing the inner part of the prostate through an incision. It is more invasive but offers the most complete and long-lasting relief.
Your healthcare provider will discuss the risks and benefits of each option to help you make an informed decision.
Understanding BPH Complications and Catheterization
Ignoring BPH symptoms can lead to serious health problems that affect more than just your bathroom routine. Understanding how BPH progresses highlights the importance of early action for your long-term health.
When an enlarged prostate obstructs urine flow, it can create a ripple effect of complications throughout your urinary system.
Potential Complications if Left Untreated
Without treatment, the constant pressure on your bladder can lead to a cascade of worsening problems.
- Acute urinary retention: A medical emergency where you suddenly become unable to urinate. It is extremely painful and requires immediate medical help to drain the bladder.
- Chronic urinary retention: The bladder never fully empties, leaving residual urine. This can weaken the bladder muscle over time.
- Recurring urinary tract infections (UTIs): Stagnant urine in the bladder creates a breeding ground for bacteria, leading to painful and repeated infections.
- Bladder stones: Minerals in concentrated, leftover urine can crystallize and form stones, causing pain, bleeding, and further obstruction.
- Bladder damage: The bladder wall can thicken and become irritable from the constant strain of pushing urine past the obstruction. Eventually, the muscle may lose its ability to contract properly.
- Kidney damage: In severe cases, urine can back up into the kidneys, causing infections and potentially permanent damage.
About half of all men with BPH will develop symptoms requiring treatment, underscoring the need to address the condition before serious complications arise.
What is BPH's Connection to Urinary Retention and Catheters?
Urinary retention is one of the most serious complications of BPH. When the enlarged prostate creates a roadblock, the bladder cannot empty properly. This is where a catheter—a thin, flexible tube inserted into the bladder to drain urine—can be a life-saving tool.
While the idea may be intimidating, many men find that catheterization restores their independence and quality of life.
- Intermittent self-catheterization is a common method for managing chronic retention. You insert a clean catheter several times a day to empty your bladder completely, then remove it. This gives you control over your schedule and relieves the discomfort of incomplete emptying.
- Foley catheters remain in place continuously, held by a small balloon inside the bladder. They are typically used in emergencies, post-surgery, or for long-term management when self-catheterization isn't feasible.
At ProMed DME, we understand that managing BPH sometimes means having the right supplies at your fingertips. We provide a comprehensive range of high-quality urology products, including various types of catheters designed for comfort and reliability. Our dedicated nurse on staff is always available to answer questions and provide guidance as you steer your treatment options.
The goal is to help you maintain your dignity, independence, and quality of life. With the right support and supplies, catheterization can be a bridge to comfort while you and your doctor determine your long-term BPH treatment plan. For more info about catheter supplies, visit our website where you'll find everything you need, backed by our commitment to exceptional customer service and support.
Frequently Asked Questions about BPH
As you learn what is BPH, it's natural to have questions. Here are answers to some of the most common concerns.
What is the difference between BPH and prostate cancer?
This is a critical distinction. BPH and prostate cancer are completely different conditions.
BPH is benign (non-cancerous). The prostate gland grows larger, but the growth does not spread to other parts of the body. Prostate cancer is malignant, meaning abnormal cells can invade other tissues and spread.
Importantly, BPH does not cause prostate cancer or increase your risk for it. However, the two conditions can exist at the same time and often cause similar urinary symptoms. This overlap is why your doctor uses diagnostic tools like the Digital Rectal Exam (DRE) and PSA blood test. While BPH can also raise PSA levels, your doctor can interpret these results in the context of your overall health.
Regular prostate cancer screening is recommended for most men between 55 and 69, or earlier for those with higher risk.
Can BPH be prevented?
There is no guaranteed way to prevent BPH, as it's largely tied to aging and hormonal changes. However, you can take steps to reduce your risk and manage symptoms.
Strategies for risk reduction include:
- Maintaining a healthy weight: Obesity is a known risk factor for BPH.
- Regular exercise: An active lifestyle can lower your risk. Aim for at least 30 minutes of moderate activity on most days.
- A balanced diet: A diet rich in fruits, vegetables, and healthy fats may support prostate health. Limiting red meat and processed foods is also beneficial.
- Managing other health conditions: Controlling heart disease, type 2 diabetes, and high blood pressure can also help reduce your BPH risk.
While you can't stop the aging process, a healthy lifestyle can significantly improve your overall quality of life and potentially lessen the impact of BPH.
Can an enlarged prostate go back to normal?
An enlarged prostate typically does not shrink back to its original size on its own. The growth is a continuous process driven by age and hormones.
However, the most important thing is that your symptoms can absolutely improve, and your urinary function can feel normal again.
- Lifestyle changes can provide significant relief for mild symptoms.
- Medications like 5-alpha reductase inhibitors (finasteride, dutasteride) can actually shrink the prostate over several months.
- Other treatments, including alpha-blockers, minimally invasive procedures, and surgery, focus on reducing the obstruction caused by the enlarged prostate, which improves urine flow even if the gland's overall size doesn't change.
The goal of treatment is to restore normal urinary function and improve your quality of life. At ProMed DME, we've seen how the right approach, whether it's medication, a procedure, or supportive care like catheter supplies, can make a transformative difference.
Conclusion: Taking Control of Your Prostate Health
Understanding what is BPH is the first step toward managing your health. The key takeaway is that BPH is incredibly common and completely manageable. You are not alone—by age 85, about 90% of men will have some degree of prostate enlargement.
The frustrating bathroom trips and sleepless nights do not have to be your new normal. From simple lifestyle changes to medications and procedures, there are proven solutions that work.
The most important step is to talk to your healthcare provider. Don't dismiss urinary symptoms as just a part of getting older. Early diagnosis and treatment can lead to simpler options and better outcomes.
If your BPH journey includes catheterization or other medical supplies, that's where we come in. At ProMed DME, we help people manage their health with dignity and confidence. We know that dealing with urological issues can be overwhelming, which is why we have a dedicated nurse on staff to answer your questions and guide you.
We make it easy by offering free shipping across the United States and working with most insurance plans to keep your costs low. Our goal is to provide you with top-quality medical supplies and the support you need to live comfortably.
Don't let BPH dictate your life. You deserve to sleep through the night and feel confident in your daily routine. Personalized care starts with taking that first step.
Take the next step in managing your health – because better days are ahead.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.