Dress for Success: Choosing the Right Burn Dressing for Every Blister

Why the Right Dressing Matters for Burn Care
Burn dressing selection can mean the difference between a quick recovery and weeks of pain, infection, or permanent scarring. With thousands of burn injuries occurring annually, choosing the right dressing is about preventing life-altering complications.
Quick Reference: Primary Goals of Burn Dressings
- Prevent infection - Create a barrier against bacteria.
- Promote healing - Maintain optimal moisture for tissue repair.
- Reduce pain - Provide cooling relief and protect nerve endings.
- Stop progression - Prevent burns from deepening.
- Enable function - Allow movement while protecting the wound.
Whether it's a kitchen scald or a serious thermal injury, the dressing directly impacts healing speed and complication risk. Research shows that proper burn dressings can reduce infection rates from 27.8% to just 9.5%. This highlights why the choice matters so much.
Different burns require different care. A first-degree sunburn needs a different approach than a blistering second-degree scald. Using the wrong dressing can slow healing, increase pain, or lead to preventable scarring.

Understanding the Injury: How Burn Depth Dictates Dressing Choice
To choose the right burn dressing, you must know which layers of skin are damaged. The deeper the burn, the more specialized the care required.
Burn classification is based on which skin layers are affected. First-degree burns damage only the outermost layer (epidermis). Second-degree burns affect the epidermis and part of the dermis. Third-degree burns are the most serious, destroying all skin layers and sometimes reaching muscle or bone.
Burns can worsen without proper care. Jackson's burn wound model explains this with three zones. The central zone of coagulation is irreversibly damaged. The surrounding zone of stasis has compromised blood flow and is at risk; the right burn dressing is critical here. The outer zone of hyperemia has increased blood flow and usually heals on its own.
Assessing severity also involves the burn's size (total body surface area), location, age, and overall health. A small burn on the hand may need more attention than a larger one on the arm due to its importance for daily function.

When to See a Doctor
When to see a doctor isn't always obvious. Seek immediate medical attention if a burn is larger than your palm, has large or broken blisters, or affects the face, hands, feet, genitals, or major joints. Chemical and electrical burns require professional evaluation, as they can cause extensive internal damage. If you've inhaled smoke or see signs of infection, don't wait.
Superficial (First-Degree) Burns
Superficial burns only affect the epidermis. A classic sunburn example shows erythema (redness) and tenderness, but no blisters. These burns don't typically require a specialized burn dressing. Focus on comfort by applying cool water for 20 minutes, followed by gentle moisturizers and emollients to soothe the skin.
Partial-Thickness (Second-Degree) Burns
Partial-thickness burns damage both the epidermis and dermis, creating blisters. Exudate management is key; the wound needs to be kept moist without becoming waterlogged. These are divided into superficial vs. deep dermal burns. A hot water scald example often causes superficial partial-thickness burns, which are painful, red, and heal within three weeks. Deep partial-thickness burns are less painful due to nerve damage, may appear white or mottled, and carry a higher risk of scarring.
Full-Thickness (Third-Degree) Burns
Full-thickness burns destroy all skin layers. Due to nerve damage, they are often painless. The white or charred skin appearance indicates the severity. These burns require medical intervention, as skin grafting is usually necessary for the skin to regenerate. A burn dressing serves as temporary protection until surgery.
The Complete Guide to Burn Dressing Types
Choosing a burn dressing is about creating the ideal healing environment: moist, protected, breathable, and comfortable. The right dressing should allow oxygen flow, keep germs out, stay in place, and reduce the frequency of painful changes.
| Dressing Type | Primary Function | Absorbency Level | Use Cases | Change Frequency | Key Advantages | Key Disadvantages |
|---|---|---|---|---|---|---|
| Hydrogel Dressings | Cooling, pain relief, rehydration | Low | Dry/sloughy burns, superficial burns, minor scalds | Daily to every 3 days | Soothing, cooling, pain relief, promotes autolytic debridement | Can dry out, may require secondary dressing, not for highly exudating wounds |
| Hydrocolloid Dressings | Moist healing, barrier, autolytic debridement | Low to Moderate | Low/moderate exudating burns, superficial partial-thickness burns, donor sites | Every 3-7 days | Waterproof, self-adhesive, conformable, good for pediatric use, long wear time | Not for infected or highly exudating wounds, can roll up at edges, opaque |
| Foam Dressings | High absorbency, cushioning | Moderate to High | Moderate/highly exudating burns, deep partial-thickness burns, hypergranulation | Every 1-3 days | Excellent absorbency, cushioning, thermal insulation, non-adherent | Can be bulky, may require secondary fixation, not for dry wounds |
| Alginate Dressings | High absorbency, haemostasis | High | Highly exudating burns, superficial bleeding areas, moist granulating wounds | Daily to every 3 days | Excellent absorbency, promotes haemostasis, biodegradable, forms gel for moist environment | Not for dry wounds, requires secondary dressing, can cause desiccation if wound is not exudating enough |
| Silver-Containing Dressings | Broad-spectrum antimicrobial, infection prevention | Variable | All burn depths (especially initially), infected/colonized wounds, where infection risk is high | Every 3-7 days | Strong antimicrobial action, reduces infection incidence, pain during changes, effective for various microbes | Can be cytotoxic to healthy cells if used too long, more costly, requires moistening |
| Biosynthetic/Biologic Dressings | Temporary skin substitutes, wound coverage | Variable | Large burn wounds, donor sites, bridge to definitive closure, especially in children | Less frequent | Reduces pain, promotes healing, reduces infection, shorter hospital stays, can stay on for longer periods | Costly, often requires clinical application, not always readily available |
Hydrogel Dressings
Containing over 96% water, hydrogel dressings provide immediate cooling relief to a burn. This burn dressing calms the injury, reduces pain, and creates a moist environment for healing. Hydrogels are ideal for painful superficial burns, like minor scalds or sunburns, and can help rehydrate dry, crusty wounds. Their cooling effect may also prevent a burn from deepening. However, they are not highly absorbent and may require a secondary dressing to stay in place.

Hydrocolloid Dressings
Hydrocolloid dressings contain gel-forming agents that interact with wound fluid to create a soft, protective gel. This burn dressing is waterproof on the outside while maintaining a moist environment against the skin. They are self-adhesive and can be left in place for up to a week, reducing painful dressing changes. This makes them a good choice for children and for moderate burns needing consistent care. Because they are opaque, the wound cannot be viewed without removal. They are not suitable for heavily draining or infected wounds.
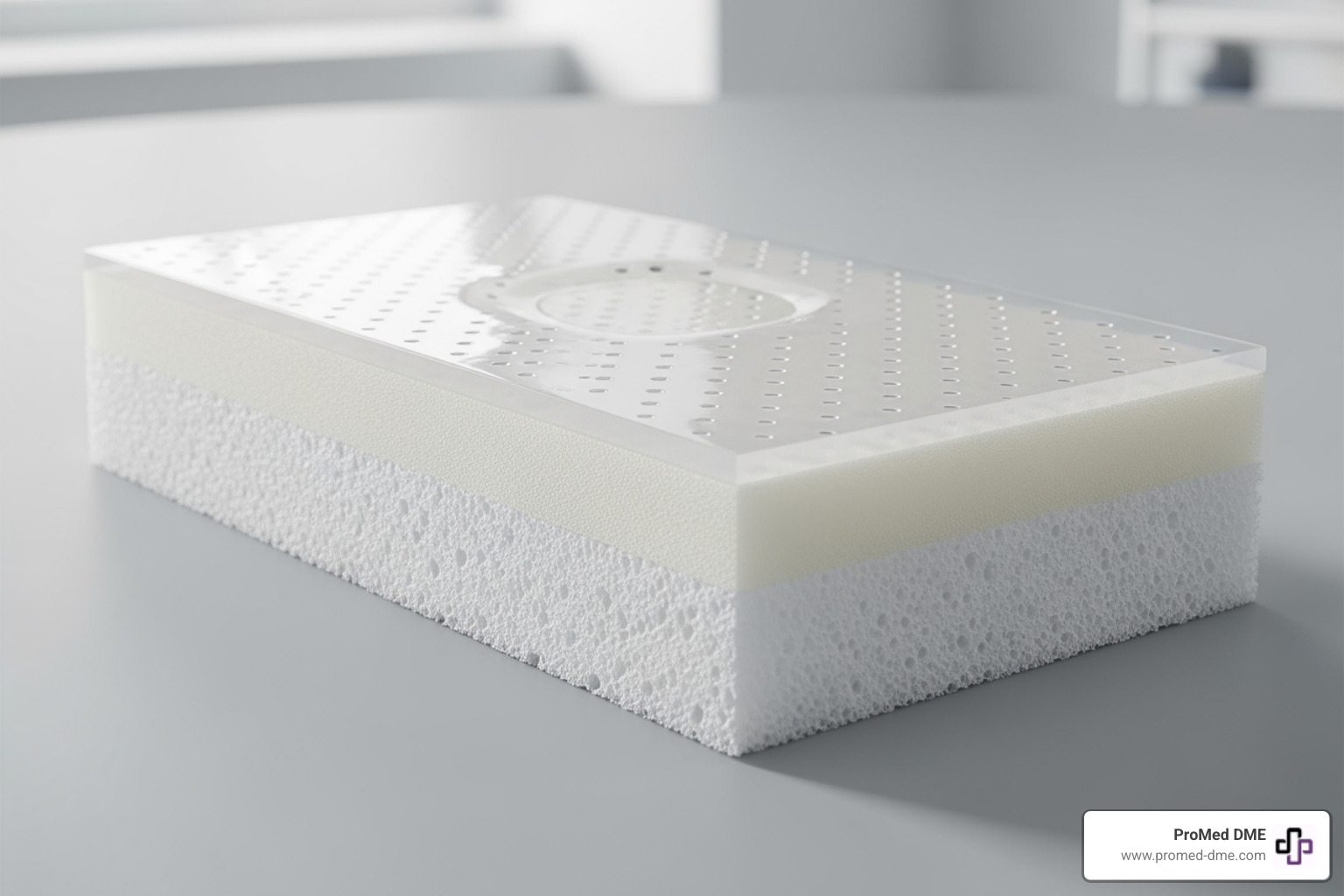
Foam Dressings
Made from soft polyurethane, foam dressings are highly absorbent and ideal for burns with significant fluid. They cushion the wound from pressure and prevent maceration (the breakdown of skin from excessive moisture). This burn dressing also provides thermal insulation, keeping the wound at an optimal temperature for healing. Their main drawback is their bulk, and they may require extra tape or bandaging to stay secure. They are not intended for dry wounds.
Alginate Dressings
Derived from brown seaweed, alginate dressings are highly absorbent and can help control minor bleeding. When the alginate fibers meet wound drainage, they form a soft gel that maintains a moist healing environment. These dressings are excellent for burns producing large amounts of fluid or those with small areas of bleeding, as the fibers naturally promote clotting. Alginates require moisture to work and must be used with a secondary dressing. They are not suitable for dry wounds.
Silver-Containing Dressings: An Antimicrobial Burn Dressing
Modern burn dressing technology uses nanocrystalline silver to fight infection. These dressings release silver ions that are toxic to a broad spectrum of bacteria and fungi. Research shows silver dressings can reduce infection rates from nearly 28% to under 10%. They are especially valuable in the first 48 hours when infection risk is highest and can cause less pain during changes than older treatments. However, prolonged use can be toxic to healthy cells, so they are best for initial treatment. They must be moistened with sterile water, not saline. You can find more information in evidence for silver dressings in wound management.
Biosynthetic and Biologic Dressings
These advanced dressings act as temporary skin substitutes, providing a scaffold for the body's healing processes. Biosynthetic and biologic burn dressing options offer immediate coverage for large or deep burns, reducing pain and fluid loss. Studies show they can reduce hospital stays, speed healing, and improve pain scores, especially in children. They can also remain in place for longer periods, meaning fewer traumatic dressing changes. Their main limitations are high cost and the need for professional application in a clinical setting.
A Step-by-Step Guide to Burn Wound Management
Proper burn wound management follows key steps to ensure the best outcome and prevent complications. Here is a guide to the process, from initial first aid to long-term care.
Initial Care: The First 48 Hours
Immediate actions after a burn are critical for the healing process.
- Stop the burning process. Move away from the heat source immediately.
- Cool the burn. Run cool (not cold) water over the area for 20 minutes. This step is proven to improve healing outcomes. Find evidence in this research on water first aid for burns. Never use ice, butter, or household ointments, which can trap heat or cause further damage.
- Remove jewelry and clothing. Gently remove any items around the burn, but leave anything stuck to the skin for medical professionals.
- Apply a dressing. Use an aseptic technique by washing your hands thoroughly before and after. For the first 48 hours, nanocrystalline silver dressings are often recommended for their antimicrobial properties. Moisten them with sterile water (not saline) and cover with a secondary dressing. The goal is to leave this initial dressing undisturbed for 48 hours.
- Manage pain. Take over-the-counter pain relievers like acetaminophen or ibuprofen before dressing changes to improve comfort.

The Blister Debate: To Debride or Not to Debride?
Whether to pop burn blisters is a common question. Blister fluid contains inflammatory substances that can restrict blood flow and worsen the burn. The blister roof is dead skin that can harbor bacteria.
Most healthcare professionals now favor removing blister fluid and loose skin. This relieves pressure, improves blood flow, and allows antimicrobial burn dressings to make direct contact with the wound bed. Intact blisters can also be painful and limit movement. Small, unbroken blisters that are not in high-friction areas might be left intact, but this decision is best made by a healthcare professional. A provider can use sterile scissors to safely remove the blister roof, reducing pain and infection risk. For more details, see this review of blister management in burns.
Ongoing Care: After the 48-Hour Mark
After 48 hours, carefully remove the initial dressing to reassess the burn. The burn dressing choice may evolve based on the wound's condition.
- For minimal fluid, a hydrogel dressing can provide cooling and moisture.
- For moderate drainage, a hydrocolloid dressing offers protection and long wear time.
- For significant fluid, an absorbent foam dressing is appropriate.
Consult a healthcare provider if the burn appears to be getting deeper, larger, or shows signs of infection. Dressing change frequency is typically every two to three days for partial-thickness burns, but follow manufacturer recommendations. Increased pain, odor, or drainage are signs that a change is needed.
Post-Healing Care: Protecting New Skin
Once the burn has healed, the new skin requires special care. It is delicate and vulnerable.
- Moisturize daily with a fragrance-free emollient to prevent dryness and itching.
- Protect from the sun. New skin is highly sensitive to UV radiation. Use a broad-spectrum sunscreen with SPF 50 or higher and avoid prolonged sun exposure for at least two years to prevent hyperpigmentation.
- Manage itching by keeping fingernails short and wearing loose-fitting clothing. If itching is severe, seek medical advice.
Advanced Topics: Scarring and Future Innovations
Even after a burn heals, complications like hypertrophic scarring can arise. This involves the formation of thick, raised, and uncomfortable scars.
Hypertrophic Scarring Risk
A burn that takes longer than 21 days to heal has a higher risk of forming problematic scars. The slow healing process can trigger an overproduction of collagen. High-risk patients, such as those with darker skin tones or a family history of keloids, require proactive management.
Scar management techniques include:
- Silicone products: Gels and sheets help flatten and soften scars by maintaining moisture.
- Pressure garments: Custom-fitted compression wear applies continuous pressure to prevent excessive collagen buildup.
- Massage and mobilization: Regular, gentle massage keeps the skin supple and prevents tightness.
- Laser therapy or surgery: These options can address severe scars that don't respond to other treatments.
Emerging Technologies
The future of burn dressing technology is rapidly advancing.
- Smart dressings are in development that can monitor a wound's condition, changing color to indicate infection or releasing medication as needed.
- Dressings are being created with embedded growth factors, stem cells, and proteins to actively accelerate healing.
- Nanotechnology is enabling tiny delivery systems that can target specific parts of the healing process.
- Enzymatic debridement agents offer a non-surgical way to remove dead tissue, preparing the wound bed for optimal healing.
These innovations promise more precise, predictable, and comfortable burn care in the future.
Frequently Asked Questions about Using a Burn Dressing
Here are answers to common questions about managing a burn dressing and caring for a burn injury.
How often should a burn dressing be changed?
The frequency depends on the dressing type and the wound's condition. Hydrocolloid dressings may stay on for up to a week, while initial silver dressings are typically changed after 48 hours. Wounds with high exudate levels (fluid) require more frequent changes to prevent skin breakdown (maceration). Always change a dressing if you see signs of infection. Follow the manufacturer's instructions and your provider's advice.
Can I put ointment or cream under a burn dressing?
Less is more. Avoid butter or household ointments, as they can trap heat and introduce bacteria. If you have prescribed topicals, follow instructions carefully; often, these are best applied to the dressing itself, not the skin, to reduce trauma during changes. Specialized dressings like hydrogels provide moisture on their own, and adding creams can interfere with their function.
When should I be concerned about infection?
Catching an infection early is critical. Contact your healthcare provider immediately if you notice any of these signs:
- Increased pain that is not relieved by medication.
- Redness spreading from the burn into healthy skin.
- A foul odor from the wound.
- Pus-like drainage (thick, yellow, green, or brown).
- A fever over 102°F (38.9°C) or one that lasts more than two days.
Conclusion: Heal Faster and Safer with the Right Support
Understanding burn dressing options is the first step toward a safer, faster recovery. The right dressing can prevent infection, promote moist wound healing, reduce pain, and stop the burn from deepening.
Matching the dressing to the wound's specific needs is practical, effective care. A dry wound may need a hydrogel, while a heavily draining wound needs a foam dressing. This knowledge, combined with proper first aid and post-healing care like using SPF 50 sunscreen, empowers you to take an active role in your recovery.
Knowing what to do gives you confidence when it matters most. However, having access to quality wound care supplies is just as important.
At ProMed DME, we know that having access to quality wound care supplies is just as important as knowing how to use them. Our dedicated nurse is always available to answer your questions about burn dressing selection or wound care techniques. We work with most insurance plans to keep your costs manageable, and we ship across the United States so you can get the supplies you need quickly.
Your healing journey deserves the right support from day one. Let us help you access the quality wound care products and expert guidance that can make all the difference in your recovery.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.