CGM Systems Explained – No More Sugar-Coating the Truth
Why Understanding Continuous Glucose Monitoring Systems Matters
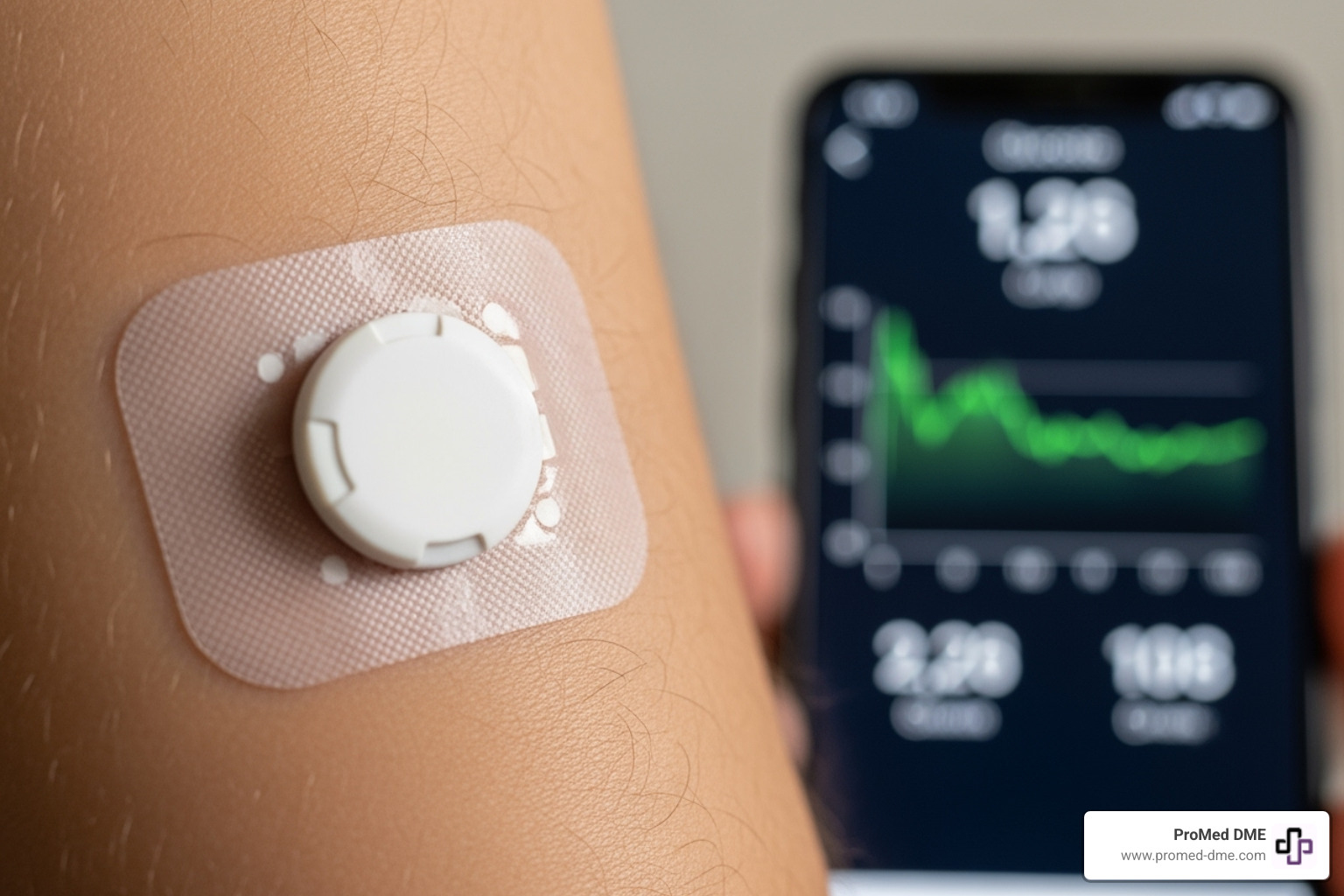
A continuous glucose monitoring system is a wearable medical device that tracks your blood sugar 24/7, reducing the need for constant fingerstick testing. Unlike traditional glucose meters that give a single snapshot, CGM systems provide real-time data and trends to help you make better decisions about your diabetes management.
Here's what you need to know about CGM systems:
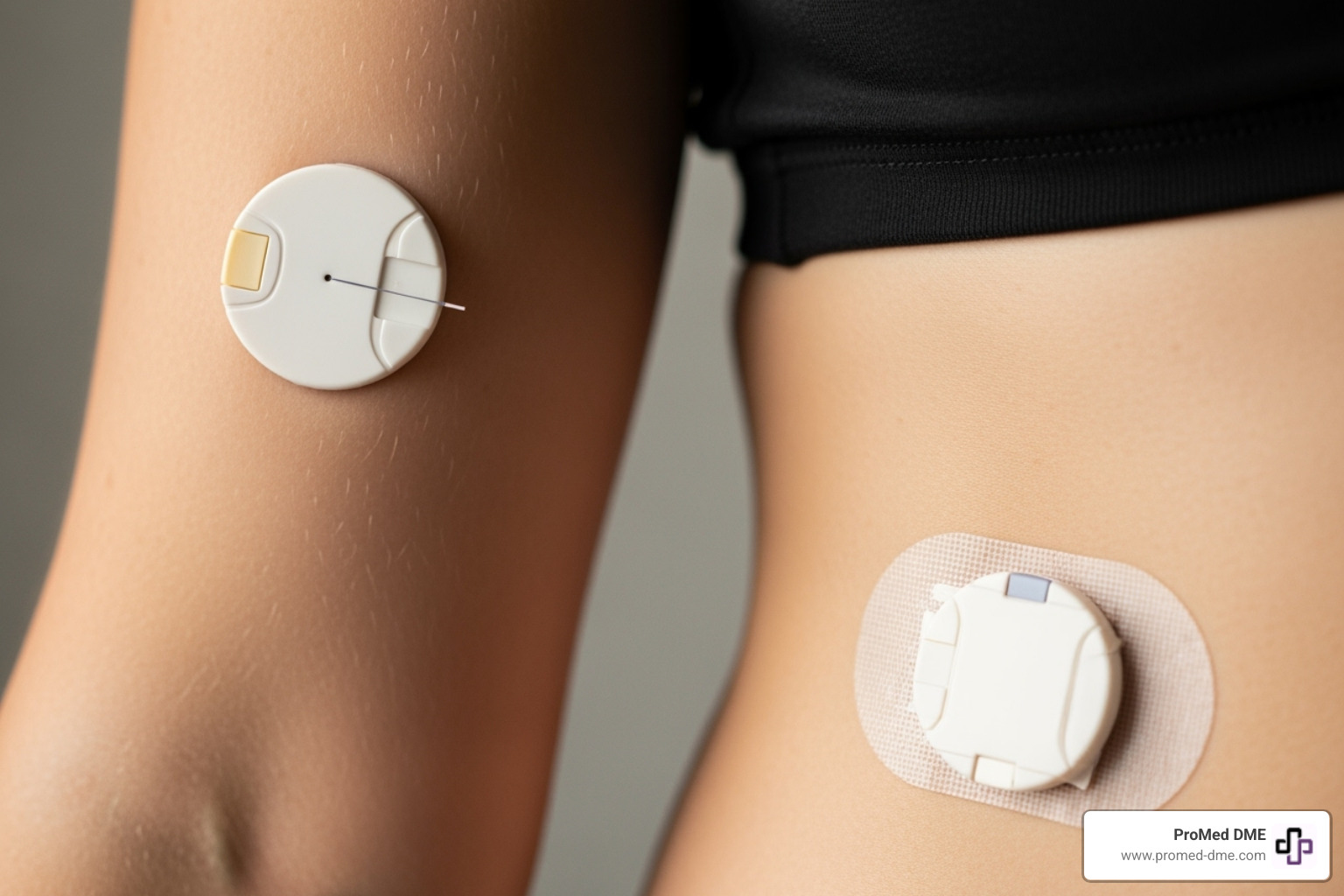
- What it is: A small sensor worn on your arm or abdomen that measures glucose in the fluid between your cells.
- How it works: The sensor sends data wirelessly to your smartphone or receiver every few minutes.
- Who benefits: People with Type 1 or Type 2 diabetes, those on insulin, and even non-diabetics interested in metabolic health.
- Key advantage: Provides continuous data instead of isolated readings, helping prevent dangerous highs and lows.
- Main components: Sensor (measures glucose), transmitter (sends data), and receiver/app (displays information).
Studies show that CGM users have fewer low blood sugar episodes and lower A1C levels compared to those using only fingerstick tests.
For many people managing diabetes, especially those on Medicare or facing insurance challenges, understanding how these systems work is the first step toward better health. The technology has evolved rapidly, with options now ranging from prescription to over-the-counter systems.
However, CGMs have costs, learning curves, and limitations to consider before making the switch.
Quick continuous glucose monitoring system terms:
What is a Continuous Glucose Monitoring System and How Does It Work?
A continuous glucose monitoring system is like a personal health assistant that never sleeps. This small, wearable medical device provides 24/7 tracking of your blood sugar, reducing the need for constant fingerstick testing.
Unlike traditional meters that give single readings, CGMs show the complete picture. They reveal glucose trends—if levels are rising, dropping, or steady. This continuous data transforms diabetes management from reactive to proactive management.
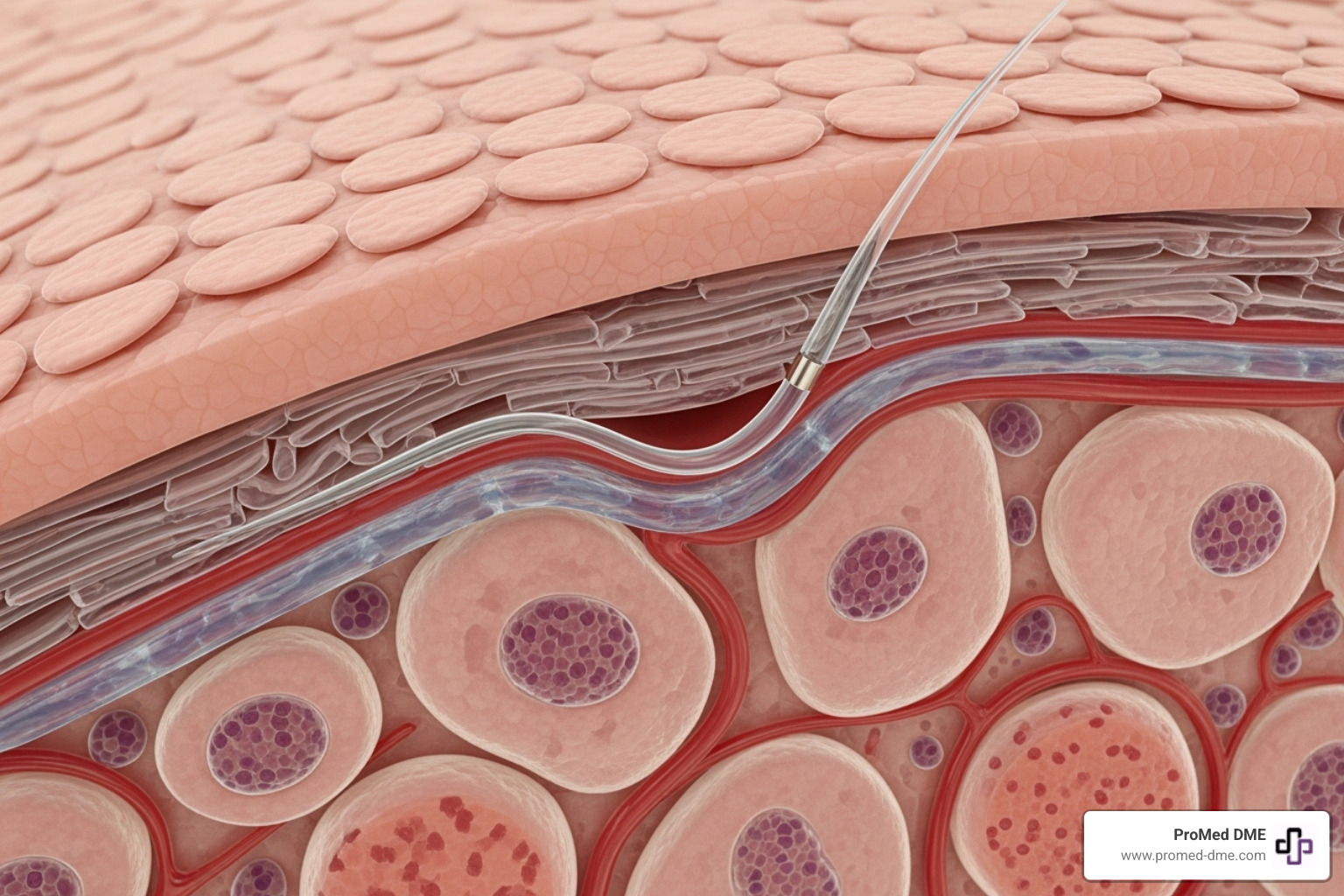
A tiny sensor under your skin measures glucose in your interstitial fluid—the liquid surrounding your cells. While not identical to blood glucose, it provides a reliable view of your body's levels.
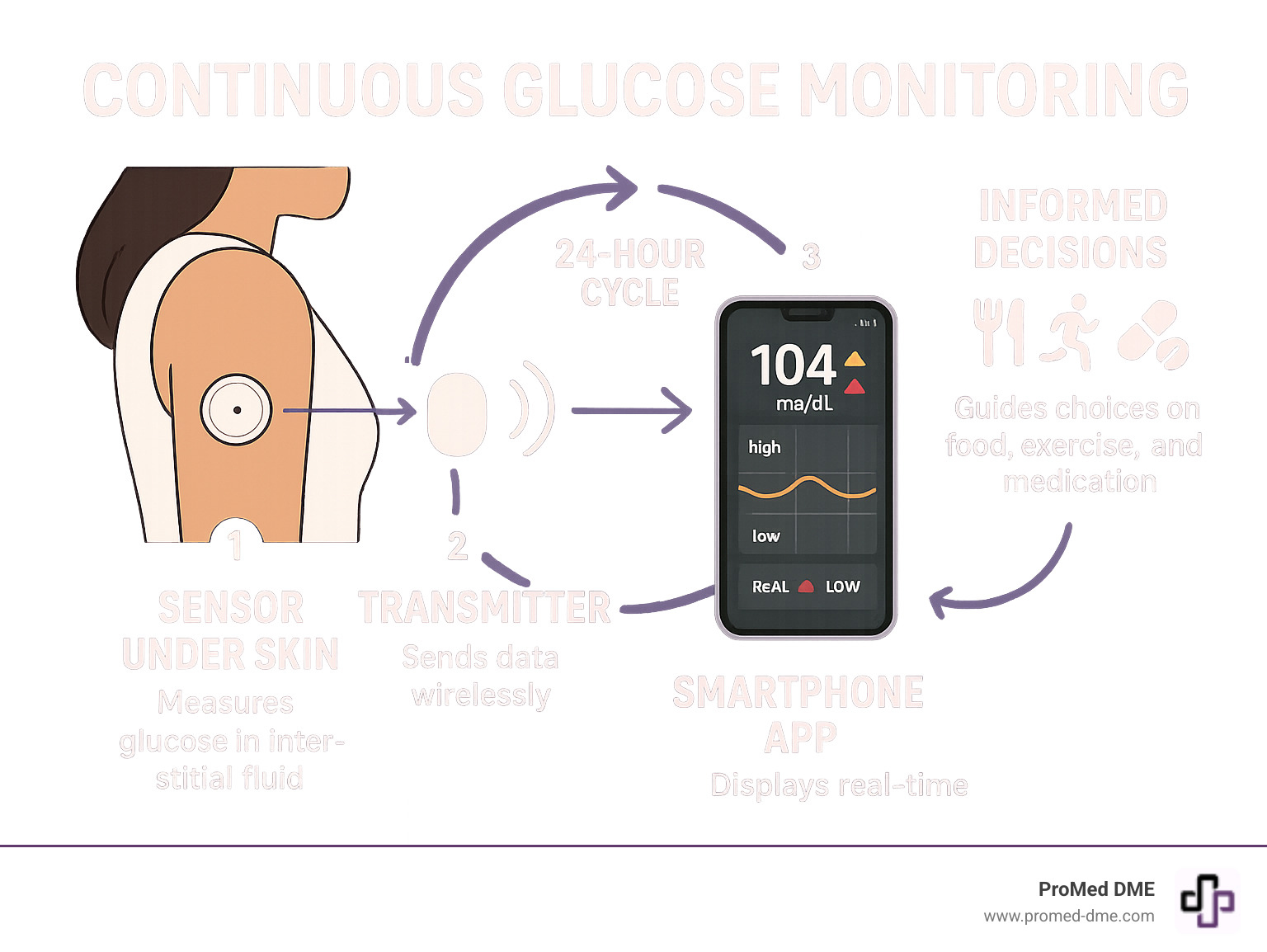
The Three Core Components of a CGM
Every continuous glucose monitoring system has three key components working together to keep you informed.
- Sensor: A tiny filament under your skin (usually on the arm or abdomen) constantly measures glucose in the surrounding fluid. Most are replaced every 7 to 14 days.
- Transmitter: This small, reusable device attaches to the sensor and wirelessly sends glucose data to your receiver. Some systems combine the sensor and transmitter into one unit.
- Receiver/Smartphone App: This is your data display—a dedicated device, phone app, or even an insulin pump. It shows your current glucose numbers, trends, and historical data.
Modern CGMs often integrate with insulin pumps for optimized management. The wireless data transmission is automatic, providing constant, up-to-date information.
Understanding the Difference: Interstitial Fluid vs. Blood Glucose
A CGM measures glucose in the interstitial fluid, not directly in the blood. This creates a lag time of 5 to 15 minutes, meaning CGM readings are slightly behind what a fingerstick blood test would show.
For daily management, this small delay is less important than the trend arrows your CGM provides. These arrows show if your glucose is rising, falling, or holding steady. Knowing the direction is often more valuable than the exact number at that moment.
CGM accuracy has improved dramatically, but it's still wise to confirm with a fingerstick test when making treatment decisions (like insulin dosing) or if a reading doesn't match how you feel. Your healthcare provider can advise when these backup checks are most important. The capillaries in your skin ensure a reliable relationship between blood and interstitial fluid glucose, making the CGM a trustworthy tool.
The Real-World Impact: Who Benefits and Why?
A continuous glucose monitoring system transforms diabetes management from reactive to proactive. This shift leads to measurable improvements in people's lives, including better sleep, less worry, and the confidence to live more fully.
Who Can Benefit from a continuous glucose monitoring system?
Modern CGM technology benefits a wide range of people beyond its initial use for Type 1 diabetes.
- People with Type 1 diabetes: Real-time data allows for precise insulin adjustments based on diet and activity, rather than guesswork.
- Those managing Type 2 diabetes: Especially for insulin users, a CGM reveals unique patterns and responses to food, stress, and exercise, providing invaluable personalized insight.
- People with Type 2 diabetes not using insulin: Can use CGM data to make impactful lifestyle changes.
- Individuals with Prediabetes: Seeing real-time feedback on how choices affect glucose can be a powerful motivator for change.
- Pregnant individuals with gestational diabetes: Benefit from constant monitoring, which helps protect both mother and baby.
- Athletes and health-conscious individuals: Use CGMs to optimize performance and metabolic health, a trend supported by the first over-the-counter CGM approval.
Key Advantages Over Traditional Fingerstick Testing
The magic of a continuous glucose monitoring system goes far beyond comfort.
- Fewer fingerpricks: This provides significant relief from the discomfort of multiple daily tests.
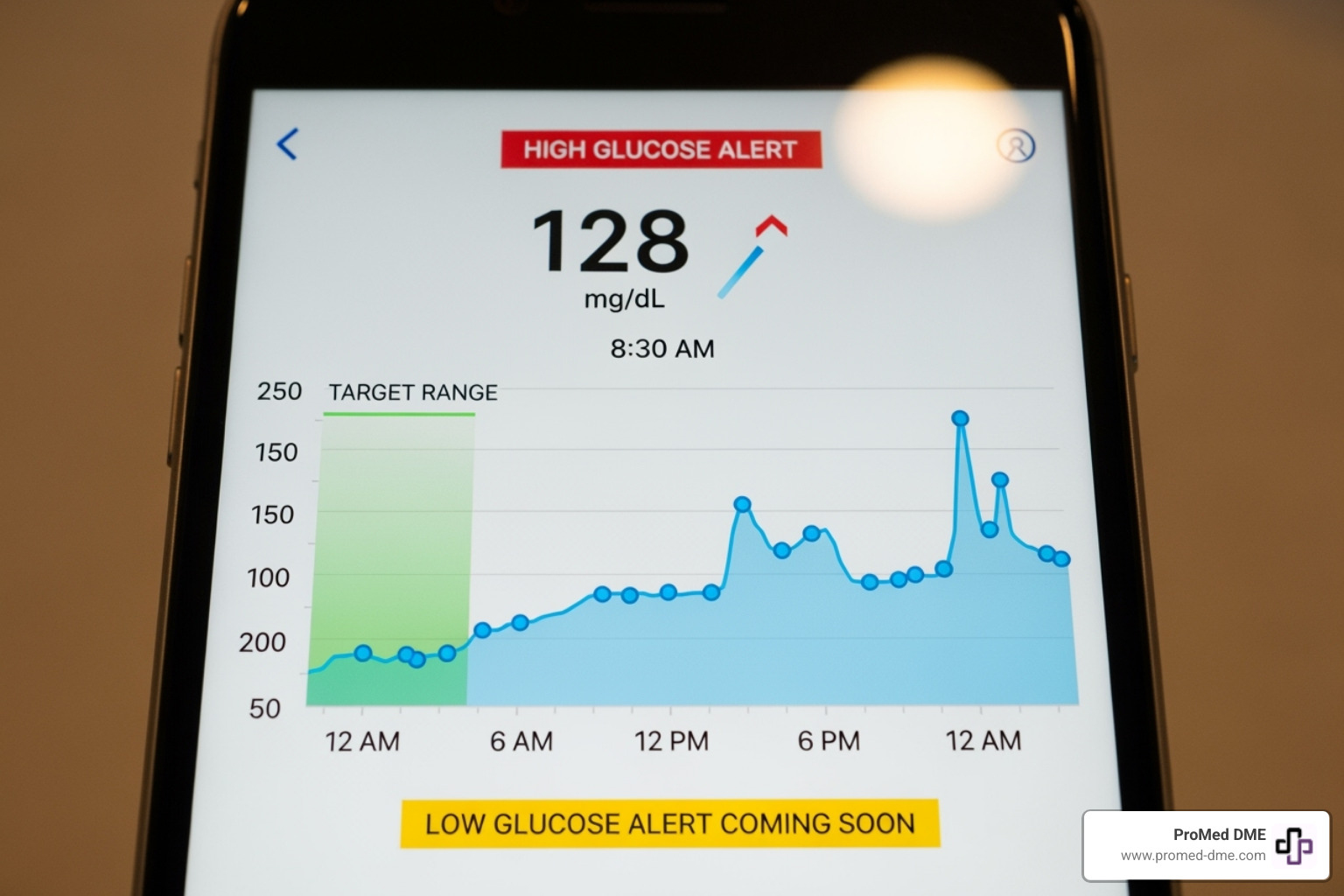
- Comprehensive data: You get a complete movie of your glucose patterns, including overnight trends that are impossible to see with fingersticks alone.
- Improved A1C levels: Research shows CGM users achieve better diabetes control, leading to improved A1C and Time in Range (TIR). Studies have shown improved well-being and decreased disease burden after 1-year use and significant reductions in HbA1c with flash glucose monitoring.
- Hypoglycemia prevention: Alerts for dropping glucose give you time to act before a dangerous low occurs, which is crucial overnight.
- Hyperglycemia alerts: Help you catch and correct high glucose levels early.
- Peace of mind: Continuous monitoring with alerts can significantly reduce the anxiety of diabetes management.
Potential Challenges and Limitations to Consider
While CGM technology is powerful, it's important to understand its challenges.
- Cost: Out-of-pocket expenses can be substantial, creating health equity issues, though insurance and Medicare coverage is improving.
- Insurance coverage: Navigating insurance can be complex. ProMed DME helps by working with most plans to minimize costs and guide you through the process.
- Accuracy concerns: There's a slight lag time since CGMs measure interstitial fluid. Certain medications like high doses of Acetaminophen (over 1000mg every 6 hours) or large amounts of Vitamin C can also affect accuracy.
- Information overload and alarm fatigue: Constant data and alarms can be overwhelming initially. Learning to interpret data and set alerts takes time and professional guidance.
- Skin irritation: Some users experience skin irritation from adhesives, requiring careful skin management.
- Learning curve: There's a learning curve to using the sensor, app, and interpreting data effectively.
Choosing and Using Your System: A Practical Guide
Choosing the right continuous glucose monitoring system is a personal journey. It's about finding a device that fits your routine and health goals, making life easier, not more complicated. The key is to find a balance where the technology helps without becoming a burden.
Always consult your healthcare provider first. They can determine if a CGM is right for you and how it will fit into your treatment plan.
How to choose a continuous glucose monitoring system
CGMs fall into two main categories. Understanding them helps you choose the best fit for your lifestyle.
- Real-Time CGMs automatically send glucose readings to your device every few minutes. They offer continuous awareness and customizable alerts for proactive management.
- Intermittently Scanned CGMs (or Flash CGMs) require you to scan the sensor to get a reading. Many newer models offer optional high and low alarms.
| Feature | Real-Time CGMs | Intermittently Scanned (Flash) CGMs |
|---|---|---|
| Data Delivery | Automatic, continuous updates to your device (every 1-5 minutes). | Requires you to scan the sensor with a receiver or smartphone to get a reading. |
| Alarms | Typically offer customizable high/low glucose alerts and predictive alarms. | Some models offer optional alarms for high/low glucose, but not always predictive. |
| User Interaction | Minimal once set up, data flows automatically. | More active user involvement (scanning required to see current data). |
| Data Sharing | Often allows real-time data sharing with caregivers or healthcare providers. | Data can be downloaded and shared, but not typically in real-time unless actively scanned. |
| Cost & Coverage | Often considered premium, but increasingly covered by insurance. | Generally more affordable, with good insurance coverage. |
The choice depends on your management style: do you prefer a constant data flow or checking in manually? Both can be effective.
Key Features to Evaluate
Consider these practical features that can impact your daily experience:
- Sensor lifespan: Most sensors last 7-14 days, while some implantable options can last up to a year.
- Warm-up time: This varies from 30 minutes to two hours before a new sensor is ready.
- Water resistance: Most CGMs allow for showering and swimming, but confirm the specifics for your activity level.
- App compatibility: Ensure the system works with your smartphone and any other health apps or insulin pumps you use.
- Data sharing capabilities: Provide an extra safety net by allowing you to share trends with caregivers and healthcare providers.
- Customizable alerts: Let you personalize alarm settings for day/night or for trends versus specific levels.
- Discreet design: A smaller, comfortable sensor is important for long-term adherence.
Navigating these choices can be overwhelming. At ProMed DME, our team helps you understand your options, work with your insurance to minimize costs, and get the right supplies delivered with free shipping. We help you find the right tools for effective health management.
The Future is Now: Advanced Diabetes Care and Access
The evolution of continuous glucose monitoring systems is reshaping diabetes care. This technology empowers patients with personalized, effective management, making the process less of a daily burden and more automated and intuitive.
The Path to an "Artificial Pancreas"
A key development from CGM technology is the "artificial pancreas," technically known as an Automated Insulin Delivery (AID) or closed-loop system. This technology is available now.
These systems combine three components: a CGM (the eyes), an insulin pump (the hands), and a smart algorithm (the brain). The algorithm uses CGM data to automatically adjust insulin delivery, mimicking a healthy pancreas. For people with type 1 diabetes, this reduces the mental burden of calculations and helps prevent dangerous highs and lows. This technology significantly reduces the daily burden of diabetes management by automating many treatment decisions.
The Reality of Access: Cost, Insurance, and Health Equity
Despite these advances, access remains a major challenge. At ProMed DME, we see how financial barriers prevent people from accessing transformative CGM technology. Without good insurance, the cost can be prohibitive, meaning access to life-saving technology can depend on a person's financial situation or location.
We're encouraged by expanding Medicare coverage for CGMs. We work directly with Medicare to help customers access supplies with minimal hassle.
However, Medicaid policies are more complex, with coverage varying by state. This disproportionately affects vulnerable populations who rely on Medicaid and face the biggest obstacles to getting this technology.
The first FDA approval of the first over-the-counter continuous glucose monitor is a step forward, but cost and lack of insurance coverage for OTC options still present equity challenges.
At ProMed DME, we're committed to bridging these gaps. We work with most insurance plans and have a dedicated nurse on staff to help you steer benefits and minimize costs. We believe everyone deserves access to this health technology. The advocacy work of organizations like the American Diabetes Association gives us hope for more uniform coverage policies.
Frequently Asked Questions About CGM Systems
Considering a continuous glucose monitoring system can bring up many questions. Based on our experience helping thousands of people, here are answers to the most common concerns.
What are the main disadvantages of using a CGM?
While CGMs are beneficial, they have some challenges:
- Cost: This can be a major hurdle without good insurance. At ProMed DME, we work with most insurance plans to help make it affordable.
- Alarm fatigue: Frequent alerts can be exhausting, but this is manageable once you fine-tune the settings with your provider.
- Information overload: It takes time to adjust to the constant stream of data.
- Skin irritation: Irritation from the adhesive can occur. Solutions like barrier wipes and rotating sites can help.
- Learning curve: It takes practice to interpret data, like trend arrows and food impacts. A diabetes educator or our on-staff nurse can help.
Do CGMs completely eliminate the need for fingerstick checks?
The short answer is no. Modern continuous glucose monitoring systems dramatically reduce the need for fingersticks, but don't eliminate them. You'll still need a backup meter for a few key situations:
- To confirm readings: If a reading seems wrong or doesn't match how you feel, a fingerstick check is crucial for safety.
- When symptoms don't match readings: Always trust your body. If you feel symptoms of high or low blood sugar but your CGM shows a normal reading, double-check with a fingerstick.
- For major medication decisions: Your provider may require a blood glucose reading for significant treatment changes, like adjusting insulin doses.
- In case of technology failure: A backup meter is essential if your CGM stops working.
You'll trade multiple daily fingersticks for occasional safety checks, which is a significant improvement.
When should I talk to my healthcare provider about my CGM?
Your healthcare provider is your partner in using your CGM effectively. Reach out to them in these situations:
- Before you start, to determine if a CGM is right for you and to get a prescription.
- To interpret data patterns that you don't understand.
- If readings consistently don't match your symptoms, to troubleshoot potential issues.
- Before making major treatment changes based on CGM data.
- For persistent skin irritation.
- To get help with insurance coverage, as their office can assist with documentation.
We're here to support you too. Our dedicated nurse can answer questions about your supplies, and we'll work with your insurance to ensure a smooth process. Managing diabetes is a team effort.
Conclusion: Taking Control of Your Metabolic Health
Understanding continuous glucose monitoring systems reveals a major shift in diabetes care: from reactive guesswork to proactive, data-driven health management. This technology fundamentally changes how we approach well-being.
A continuous glucose monitoring system acts as a 24/7 health assistant. This constant stream of personalized data empowers you to make informed decisions about meals, exercise, and medication that were previously impossible.
The benefits—improved glycemic control, reduced hypoglycemia risk, better A1C levels, and increased time in range—all lead to a better quality of life. Anticipating trends gives you a powerful sense of control and confidence.
The path forward isn't always simple. Challenges like insurance and a learning curve exist. However, the initial adjustment is worthwhile. With support from a healthcare team, a CGM can become an invaluable tool.
At ProMed DME, we've seen this technology change lives. Getting started requires a partner to help steer insurance, answer questions, and ensure you get supplies on time. That's why we work with most insurance plans, offer free shipping across the United States, and have a dedicated nurse on staff ready to support you.
Your health journey is unique. The right continuous glucose monitoring system should fit your life seamlessly. This technology offers unprecedented insight for anyone managing diabetes or seeking to optimize their metabolic health.
The future of diabetes care is here and more accessible than ever, with over-the-counter options and artificial pancreas systems leading the way toward automated, personalized management.
Ready to take the next step? Visit https://www.promed-dme.com to learn more about how we can support you with top-quality products and the exceptional customer service that sets us apart. Let's work together to make your continuous glucose monitoring system journey as smooth and successful as possible.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



