Your Go-To Guide for Locating Durable Medical Equipment Providers

Why Finding the Right DME Provider Matters for Your Health and Budget
A dme provider is a Medicare-approved supplier that delivers durable medical equipment (DME) like wheelchairs, oxygen machines, and CPAP devices to patients at home. When managing a chronic condition, the right provider becomes a healthcare partner, helping with insurance, patient education, and ongoing support.
Quick Guide to Finding DME Providers:
- Medicare-approved suppliers: Use Medicare.gov's supplier directory tool
- Check accreditation: Look for ACHC or Joint Commission certification
- Verify insurance participation: Ensure they accept Medicare assignment
- Product specialization: Choose providers that focus on your specific needs
- Local vs. national: Consider delivery options and customer support
However, not all DME providers are the same. Some specialize in respiratory equipment, while others focus on mobility aids. Understanding Medicare's specific coverage rules is also crucial, as it can save you hundreds in out-of-pocket costs.
This guide will walk you through finding and working with DME providers. You'll learn how Medicare coverage works, what to ask potential suppliers, and how to avoid common billing issues.
Basic dme provider vocab:
Understanding DME and Medicare Coverage
When your health requires medical equipment at home, understanding how Medicare works with a dme provider can save you money and stress. Medicare Part B is your primary coverage for durable medical equipment, but it has specific rules about what qualifies and what you'll pay. Once you know the basics, the process becomes much more straightforward.
What Qualifies as Durable Medical Equipment (DME)?
For Medicare to cover equipment, it must meet several criteria. It must be:
- Durable: Able to withstand repeated use over time.
- Medically Necessary: Used for a medical reason, not just for convenience.
- For the Sick or Injured: Primarily useful only to someone with a medical condition.
- For Home Use: Appropriate for use in your home.
- Long-Lasting: Expected to last for at least 3 years.
These rules ensure that Medicare resources are used for necessary medical equipment that offers long-term value.
Common Types of DME Covered by Medicare Part B
Medicare Part B covers a wide range of equipment when prescribed by your doctor and deemed medically necessary. Mobility aids like walkers, wheelchairs, and scooters help people maintain independence. Hospital beds with adjustable features can be covered for conditions requiring specific positioning.
For respiratory conditions, CPAP machines and oxygen equipment are commonly covered, along with related supplies. People with diabetes can get coverage for blood glucose monitors, test strips, and lancets through their dme provider.
Other covered items include nebulizers for breathing conditions, patient lifts for safe transfers, and basic items like canes, crutches, and commode chairs when medically necessary.
Your doctor and dme provider can help determine which items qualify for coverage based on your medical condition.
What Medicare Does NOT Cover
Understanding what Medicare doesn't cover as DME can prevent surprises. Convenience items that aren't medically necessary typically don't qualify.
Home modifications like ramps, widened doorways, grab bars, raised toilet seats, and stair lifts also fall outside DME coverage, as Medicare classifies them as home improvements rather than medical equipment.
Disposable supplies like bandages, gauze, or adult diapers don't meet the durability requirement. However, some disposable supplies directly related to covered DME—like replacement masks for CPAP machines—might be included. When in doubt, ask your dme provider about coverage before ordering.
Eligibility and Costs for Medicare DME Coverage
To get Medicare coverage for DME, you need a prescription from a Medicare-enrolled doctor documenting that the equipment is medically necessary for home use.
Once you have a prescription, the cost structure is straightforward. You must first meet your annual Medicare Part B deductible. After that, you typically pay 20% of the Medicare-approved amount, while Medicare covers the other 80%.
The Medicare-approved amount is what Medicare deems a reasonable payment. When your dme provider accepts Medicare assignment, they agree to accept this amount as full payment, which saves you money.
Renting versus buying depends on the equipment and your needs. Most DME starts as a rental. For long-term use, some items can be purchased, and others may become yours after a set number of rental payments. Your dme provider will explain the most cost-effective option for your situation.
How to Find and Choose the Right DME Provider
Finding the right dme provider is about choosing a long-term healthcare partner who understands your needs, works with your insurance, and provides genuine support. Not all providers are the same; some prioritize speed, while others focus on patient education and ongoing care. Choosing a great provider helps you confidently manage your health at home.
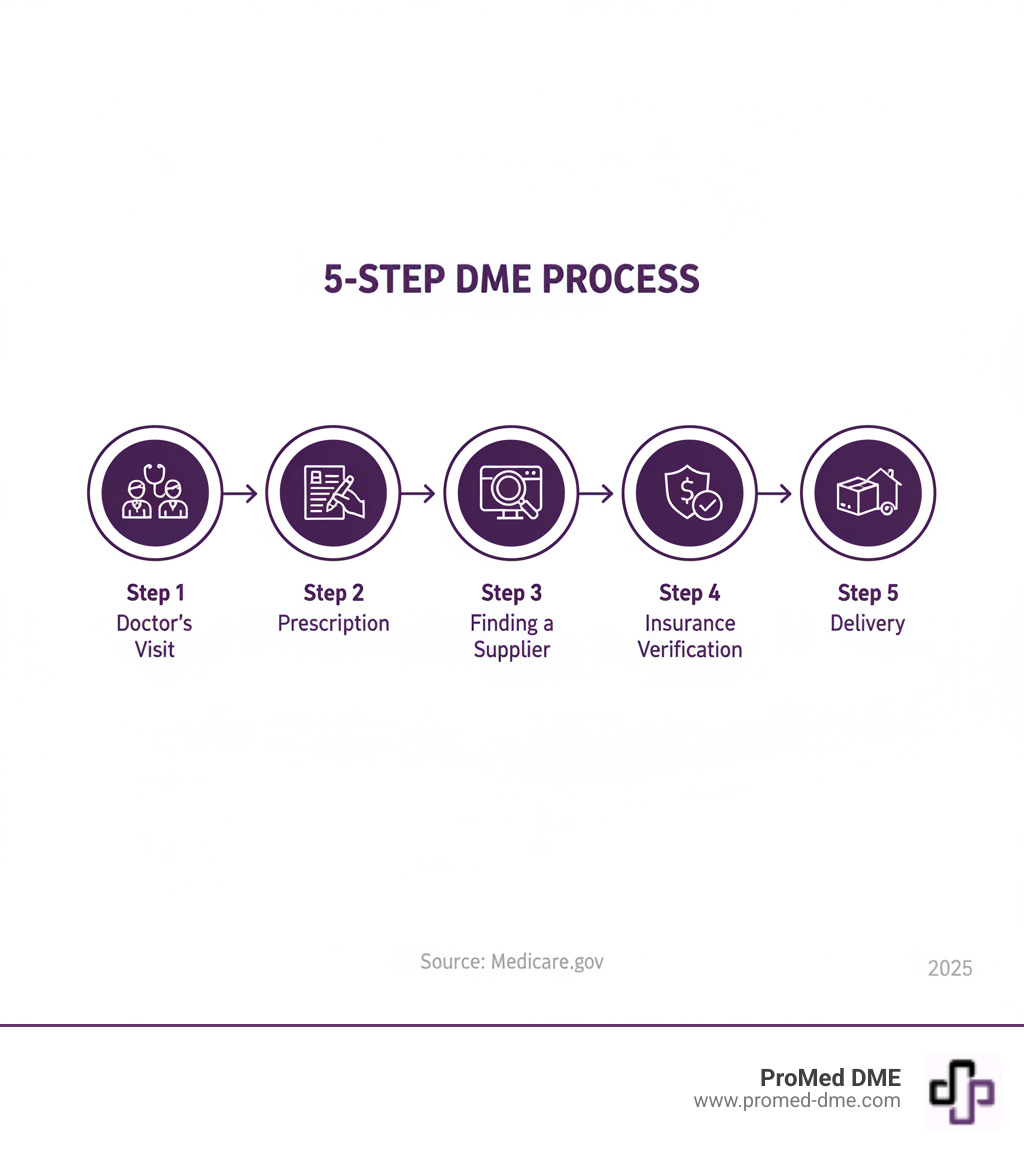
Steps to Find a Medicare-Approved DME Supplier
Your first step is ensuring any dme provider you consider is approved by Medicare, which is essential for insurance coverage.
Start by visiting Medicare.gov and using their Supplier Directory tool. Simply enter your zip code to get a list of nearby suppliers enrolled with Medicare. Every legitimate supplier has a Medicare Supplier Number, which proves they can bill Medicare and meet its quality standards.
You can also filter your search by the type of equipment you need, such as a wheelchair or oxygen equipment. This narrows down the results so you only contact providers who carry what you need.
Key Factors for Choosing a DME Provider
Once you have a list of Medicare-approved suppliers, it's time to choose the right one for your needs.
- Accreditation: Look for providers accredited by organizations like the Accreditation Commission for Health Care (ACHC) or The Joint Commission. This is a seal of approval indicating high standards for patient safety and service.
- Insurance Participation: Confirm they accept Medicare and participate with your specific plan, especially if you have a Medicare Advantage plan.
- Product Specialization: A provider specializing in your needed equipment (e.g., respiratory, mobility, wound care) often provides better product selection and more knowledgeable support.
- Patient Reviews: Look up online reviews and ask your doctor for recommendations. Real patient experiences reveal a lot about customer service and reliability.
- Delivery and Setup: Quality delivery and setup services, including training on how to use the equipment, can make a significant difference in your daily life.
The Benefits of a Supplier That Accepts Medicare Assignment
Choosing a dme provider that accepts Medicare assignment is crucial for your budget. This agreement protects you from surprise costs.
- Cost Savings: The provider agrees to accept Medicare's approved amount as full payment. You'll only pay your Part B deductible and 20% coinsurance, with no extra charges.
- Direct Billing: The provider bills Medicare directly, saving you from paying upfront and filing for reimbursement.
- Simpler Process: This lets you focus on your health instead of wrestling with insurance claims.
If a provider doesn't accept assignment, they can charge more than Medicare's approved amount, and you might have to pay the full cost upfront. Always ask about assignment before committing.
The DME Billing and Ordering Process Explained
Getting your medical equipment shouldn't feel like solving a puzzle, but let's be honest - the paperwork can be overwhelming. Understanding how the billing and ordering process works will help you avoid delays and unexpected costs. Think of this as your roadmap to getting the equipment you need without the headaches.

The Role of a Prescription and Medical Necessity
Everything starts with your doctor - and we mean everything. Without the right prescription and documentation, even the best dme provider can't help you get coverage from Medicare.
Your Medicare-enrolled doctor needs to write a doctor's order that clearly states why you need the specific equipment. This isn't just a casual note - it needs to confirm that the equipment is medically necessary for your condition and will be used in your home.
For more complex equipment, your doctor will need to complete a Certificate of Medical Necessity (CMN). Think of this as the detailed explanation that tells Medicare exactly why you need that oxygen concentrator or hospital bed. It includes your diagnosis, how the equipment will help, and other medical details that justify the expense.
Many items also require a Detailed Written Order (DWO). This goes beyond the basic prescription to include specifics like what type of equipment you need, how often you'll use it, and how long you'll need it. For example, if you need oxygen therapy, the order will specify how many liters per minute you require.
Your doctor's office will also need to provide supporting medical records that back up the prescription. These records help Medicare understand your condition and why the equipment is essential for your care. Without this documentation trail, your claim will likely be denied, no matter how legitimate your need.
How DME Claims are Billed to Medicare
Once your doctor provides all the necessary paperwork, your dme provider takes over the complex world of Medicare billing. Here's how the process typically unfolds.
First, your provider assigns specific HCPCS Level II codes to your equipment. These codes are like a universal language that tells Medicare exactly what you're receiving - whether it's a basic walker or a sophisticated CPAP machine. Getting these codes right is crucial for proper billing.
Next comes submitting the claim to Medicare. Your provider bundles together all the documentation - your prescription, medical records, and proper codes - and sends it to Medicare for review. If your provider accepts assignment (which we always recommend), they handle this entire process for you.
Medicare then reviews everything to make sure all requirements are met. They're checking that the equipment is medically necessary, properly coded, and prescribed by an enrolled provider. This review process can take some time, which is why starting early is always wise.
Finally, there's your patient responsibility. After Medicare approves the claim and pays their 80%, you'll be billed for your Part B deductible (if you haven't met it yet) and your 20% coinsurance. A good provider will verify your insurance coverage before delivery, so you'll know what to expect.
The best dme provider companies understand the complexities of Information on DMEPOS supplier enrollment, which ensures they meet all Medicare requirements to serve you properly. This knowledge makes the difference between a smooth experience and a frustrating one filled with claim denials and delays.
A Look at Different Types of DME Providers
The world of dme provider options is varied. Understanding the differences between provider types helps you find the perfect match for your needs.

National Distributors vs. Local Suppliers
You'll encounter two main types of dme provider companies: large national distributors and smaller local suppliers.
National distributors operate extensive networks, delivering equipment across the country. They typically have massive inventories, ensuring they have what you need, and offer efficient logistics, including next-day delivery. Their size can lead to competitive pricing and reliable service, making them a solid choice for predictable needs.
Local suppliers offer a personal touch and customized care. They build relationships with patients and often excel at hands-on support, such as in-home setup and training. This personalized service can be invaluable, especially when you need immediate assistance or have unique requirements.
Specialized vs. General DME Providers
Beyond size, dme provider companies also differ in their focus.
Specialized providers are experts in specific fields, such as respiratory care or mobility. A respiratory-focused provider may have therapists on staff to fine-tune CPAP settings, while a mobility specialist can offer custom wheelchair fittings. Their deep knowledge is beneficial for complex conditions requiring specialized equipment.
General providers offer a "one-stop-shop" approach, stocking everything from wheelchairs to wound care supplies. This breadth is convenient if you have varied or changing health needs, as you can manage everything through a single relationship. This simplifies billing, communication, and delivery coordination.
What to Expect: Services and Support
A good dme provider should do more than just deliver equipment. Key services include:
- Patient Education: Ensuring you are comfortable and knowledgeable about using and maintaining your equipment.
- Round-the-Clock Support: Offering 24/7 assistance, especially for life-sustaining equipment like oxygen concentrators.
- Repair and Maintenance: Providing fast, reliable repair services and preventive maintenance to keep your equipment running smoothly.
- Insurance Assistance: Handling insurance verification, prior authorizations, and helping you understand your coverage to minimize out-of-pocket costs.
- Clinical Staff Access: Providing access to a nurse or respiratory therapist to answer medical questions related to your equipment.
The best providers become partners in your healthcare journey, understanding that behind every order is a person managing their health at home.
Frequently Asked Questions about DME Providers
We know navigating durable medical equipment can raise plenty of questions. That's perfectly normal! After helping thousands of patients over the years, we've noticed the same questions come up time and again. Let's tackle the most common ones to help clear up any confusion.
What is the difference between a DME provider and a DME supplier?
This is one of those questions where the answer seems obvious until you really think about it. While many people use these terms interchangeably, there's actually a meaningful difference that's worth understanding.
Your DME provider is typically your doctor, physical therapist, or another healthcare professional. They're the ones who examine you, assess your medical needs, and determine what equipment would help improve your quality of life. Think of them as the prescriber - they provide the medical justification and write the order that makes everything possible.
A DME supplier, on the other hand, is the company that actually gets the equipment to your door. They handle everything from maintaining inventory to coordinating with your insurance company to setting up your equipment in your home. The supplier supplies, while the provider prescribes.
Both roles work together to ensure you get the right equipment at the right time. Your doctor identifies what you need, and your dme provider company makes it happen. It's a partnership that puts your health and comfort first.
How do I ensure my DME supplier is properly accredited?
Nobody wants to worry about whether their medical equipment supplier meets proper standards. The good news is that checking accreditation is straightforward once you know where to look.
Start with Medicare's supplier directory at Medicare.gov. This official government tool only lists suppliers who are enrolled with Medicare, which is your first quality checkpoint. But don't stop there.
Look for accreditation from respected organizations like the Accreditation Commission for Health Care (ACHC) or The Joint Commission. These groups have strict standards for quality, safety, and patient care. Many reputable suppliers proudly display their accreditation certificates on their websites or in their offices.
Don't feel awkward about asking directly about accreditation status. Any quality dme provider will be happy to share this information. In fact, they should be proud to talk about their certifications. If a supplier seems hesitant or can't provide clear answers about their accreditation, that's a red flag worth paying attention to.
What's the difference between medical supplies and durable medical equipment?
This distinction trips up a lot of people, especially when it comes to understanding what Medicare will and won't cover. The key difference comes down to how long the item lasts and how it's used.
Durable Medical Equipment is built to last at least three years with regular use. We're talking about items like wheelchairs, hospital beds, oxygen concentrators, and CPAP machines. These are substantial pieces of equipment that become part of your daily routine for managing a chronic condition or recovering from an injury.
Medical supplies, however, are the consumable items you use up and replace regularly. Think bandages, test strips for diabetes monitoring, catheter supplies, or ostomy bags. These items serve an important medical purpose, but they're designed to be used once or for a short period before being replaced.
Here's where it gets interesting for your wallet: Medicare Part B typically covers DME when it's medically necessary and prescribed by your doctor. Medical supplies have different coverage rules, and some may not be covered at all under Medicare Part B. However, supplies that are directly related to covered DME equipment - like masks and tubing for your CPAP machine - often are covered.
Understanding this difference helps you have more realistic expectations about coverage and costs when working with your dme provider. It also explains why your supplier might handle billing differently for various items you receive.
Conclusion
Getting the right durable medical equipment doesn't have to feel overwhelming. Throughout this guide, we've walked through the essential steps together - from understanding what qualifies as DME to finding a trusted dme provider who truly cares about your needs.
The most important thing to remember? You have the power to make informed choices that can save you money and improve your quality of life. When you work with a Medicare-approved supplier who accepts assignment, you're protecting yourself from unexpected costs. When you choose an accredited provider with clinical staff support, you're ensuring someone will be there to help when questions arise.
Your doctor's prescription is your starting point, but finding the right partner to fulfill that prescription makes all the difference. Whether you need a CPAP machine for better sleep, a wheelchair for improved mobility, or diabetes supplies for daily management, the right dme provider becomes part of your healthcare team.
We know that dealing with chronic health conditions is challenging enough without worrying about equipment failures, insurance headaches, or confusing billing. That's why choosing a provider who offers comprehensive support - from patient education to 24/7 technical assistance - can transform your experience from stressful to seamless.
At ProMed DME, we've built our entire approach around making your life easier. Our dedicated nurse is always available to answer your clinical questions, and we handle the insurance paperwork so you don't have to. We believe that exceptional customer service isn't just a nice-to-have - it's essential when you're managing your health at home.
From our base in Stuart, Florida, we ship quality urology, diabetes, wound care, and bracing products across the United States. Free shipping and working with most insurance plans means fewer surprises and more focus on what matters most - your health and comfort.
Your journey with durable medical equipment should feel supported, not overwhelming. When you're ready to experience the difference that genuine care and clinical expertise can make, we're here to help.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



