Is an Insulin Pump Right for Elderly Patients? A Comprehensive Guide

Why Insulin Pump Technology Matters for Aging Adults with Diabetes
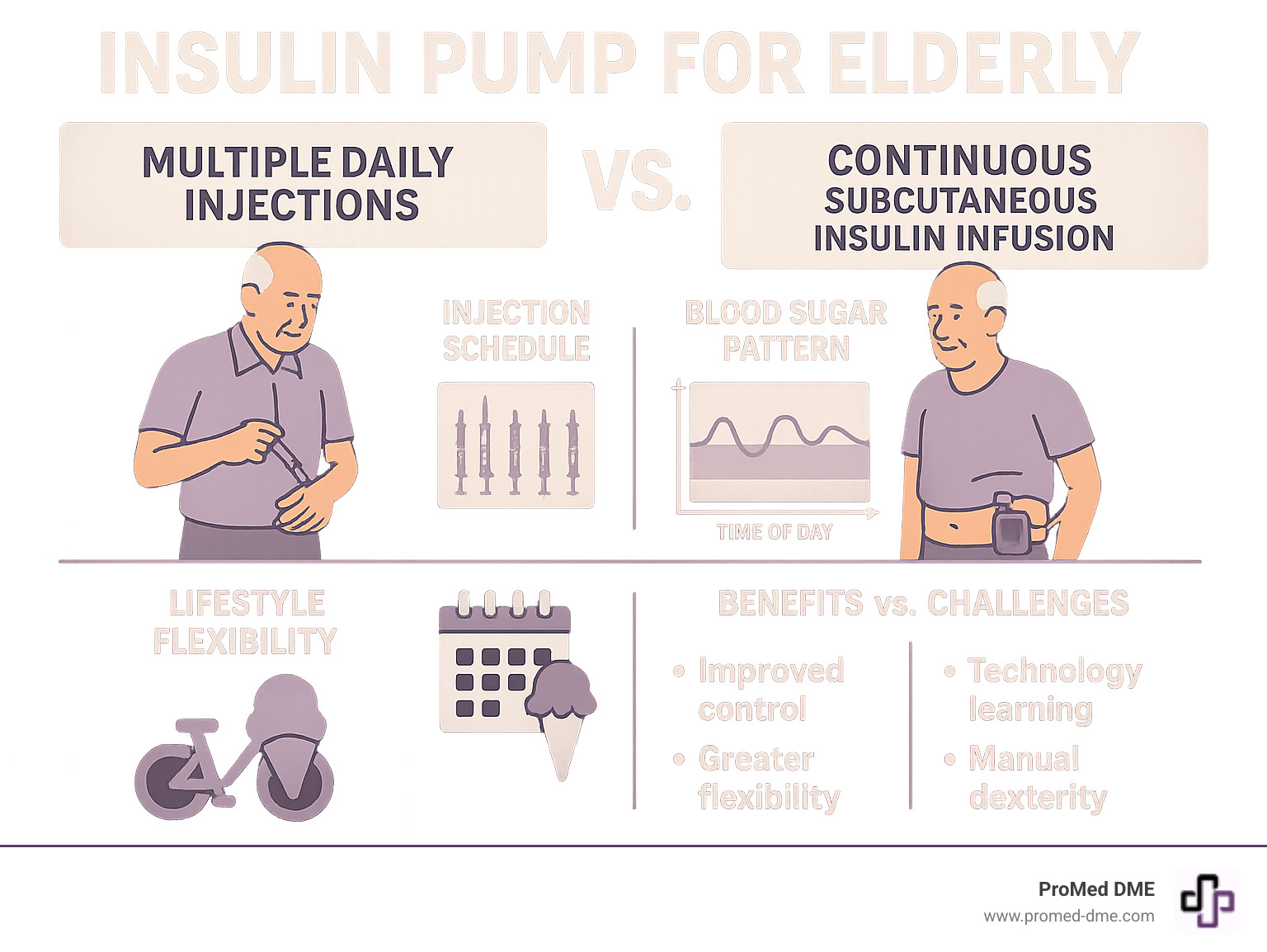
Insulin pump for elderly patients can be a game-changing treatment, but it's not right for everyone. With over a quarter of adults aged 65+ living with diabetes, it's crucial to understand this technology. Key considerations include:
- Effectiveness: Research shows pumps are as effective and safe in patients over 50 as in younger adults.
- Benefits: They offer improved blood sugar control, fewer severe low blood sugar events, and greater lifestyle flexibility.
- Challenges: A technology learning curve, manual dexterity needs, and the necessity of strong support systems are real problems.
- Coverage: Medicare covers pumps for Type 1 diabetes, but requires quarterly doctor visits for supplies.
- Candidacy: Ideal for motivated patients with adequate vision, dexterity, and caregiver support.
Modern pumps offer features like smartphone control and automated insulin adjustments that can significantly improve quality of life. Studies show older adults on advanced systems can achieve 75% time in healthy blood sugar ranges. However, the decision isn't just about technology; it's about matching the right tool to the individual's abilities and goals. This guide will help you steer the practical considerations of using an insulin pump as an older adult.
Insulin pump for elderly word roundup:
- aace guidelines for insulin pump therapy
- advantages and disadvantages of insulin pump therapy
- continuous glucose monitoring system
Understanding Insulin Pumps and How They Work
If you're considering an insulin pump for elderly diabetes management, it helps to understand what these devices do. An insulin pump is a small, computerized device that takes over the job your pancreas can no longer do effectively.
The Basics of Insulin Pump Therapy
An insulin pump delivers insulin through Continuous Subcutaneous Insulin Infusion (CSII), replacing multiple daily injections. It mimics a healthy pancreas by providing insulin in two ways:
- Basal Rate: A continuous, slow trickle of rapid-acting insulin throughout the day and night. This rate can be programmed to change at different times to match your body's needs.
- Bolus Dose: An extra dose of insulin you take for meals or to correct high blood sugar. You input your carbohydrate intake, and the pump's built-in calculator determines the correct dose.
The insulin is delivered via a thin tube called a cannula, which is part of an infusion set that you place just under the skin and change every two to three days. This system provides precise, around-the-clock insulin delivery that closely matches your body's natural rhythm.
Tubed vs. Tubeless (Patch) Pumps

When choosing an insulin pump for elderly patients, a key decision is between tubed and tubeless (patch) pumps.
Tubed pumps are the traditional style. The device clips to your clothing or sits in a pocket, connected by a thin tube to the infusion set on your skin.
- Pros: They often hold more insulin, may have easier-to-use physical buttons, and can be temporarily disconnected for activities like showering.
- Cons: The tubing can sometimes get caught on objects, which may be a concern for those with mobility or vision challenges.
Tubeless pumps (patch pumps) are a single pod that sticks directly to your skin, combining the reservoir, pump, and infusion set. You control it wirelessly with a handheld device or smartphone.
- Pros: They are very discreet, have no tubing to manage, and are often fully waterproof, allowing for swimming and showering without disconnection.
- Cons: They typically hold less insulin (requiring more frequent pod changes) and the smaller size may be difficult for those with dexterity issues.
Both types are effective. The best choice depends on your lifestyle, physical abilities, and personal preference.
Benefits and Challenges of Insulin Pumps for Seniors
Deciding on an insulin pump for elderly patients requires weighing the significant advantages against the potential difficulties.
Key Advantages for Older Adults
Research shows compelling benefits for older adults using insulin pumps, improving both health and quality of life.
- Better Blood Sugar Control: Studies show older adults on advanced pumps can spend 75% of their time in a healthy blood sugar range (Time in Range), with minimal time spent in dangerously low ranges. Research confirms pump therapy is as effective for older users as it is for younger ones.
- Reduced Severe Hypoglycemia: The fear of dangerously low blood sugar, which can cause falls or confusion, is a major concern for seniors. Pumps integrated with Continuous Glucose Monitors (CGMs) have been shown to reduce severe hypoglycemic events by up to 90%.
- Fewer Needle Sticks: Replacing multiple daily injections with an infusion set change every 2-3 days is a significant relief for many, reducing needle anxiety and the daily burden of injections.
- Greater Lifestyle Flexibility: Pumps allow you to eat when you're hungry, not when an injection schedule dictates. You can easily adjust insulin for exercise, spontaneous meals, or longer dinners, providing a sense of freedom.
Scientific research on pump effectiveness in older adults confirms that the safety and benefits of pump therapy hold steady across age groups, offering confidence in this treatment option.
Potential Drawbacks and Considerations
Honest discussion about challenges is key to success. Potential drawbacks include:
- Technology Learning Curve: Modern pumps are sophisticated. For seniors less familiar with digital devices, the learning process can feel steep, though comprehensive training helps build confidence.
- Physical and Cognitive Requirements: Using a pump requires adequate manual dexterity for changing sets, good vision for reading screens, and sound cognitive function for making decisions and troubleshooting. Any decline in these areas must be carefully evaluated for safety.
- Skin Sensitivity: Adhesives on infusion sets and patch pumps can irritate older, more fragile skin. Proper site rotation and skin care are essential.
- Risk of Diabetic Ketoacidosis (DKA): Pumps use only rapid-acting insulin. Any interruption in delivery (e.g., a kinked tube or dislodged site) can lead to DKA more quickly than with injection therapy, as there is no long-acting insulin backup.
- Cost and Supply Access: Even with Medicare coverage, navigating supply acquisition can be difficult. A survey showed over 50% of older users faced supply challenges, leading to risky workarounds. At ProMed DME, we help steer insurance and prevent supply gaps.
Is an Insulin Pump for Elderly Patients the Right Choice?
Deciding on pump therapy requires honest conversations with your healthcare team and family. Both pumps and multiple daily injections can lead to successful diabetes management; the goal is to find the best fit for your life.
Who is an Ideal Candidate?
Successful pump users, regardless of age, are typically:
- Motivated: Genuinely interested in learning a new way to manage their diabetes.
- Struggling with Injections: People with Type 1 or Type 2 diabetes on multiple daily injections who aren't meeting their blood sugar goals.
- Seeking Flexibility: Individuals who want more freedom around meal times and daily activities.
- Well-Supported: Patients with a strong support system, such as a spouse, family member, or friend who can learn alongside them and assist when needed.
Essential Factors for an elderly person to Consider Before Starting
Your healthcare team will perform a "readiness check" before you start. Key evaluation points include:
- Cognitive Function: Can you remember tasks, respond to alarms, and make dosing decisions? If not, a dedicated caregiver is essential.
- Manual Dexterity: Are you able to handle small buttons and change infusion sets? Tubeless pumps may be an option for those with arthritis.
- Vision and Hearing: Is your sight and hearing sufficient to read the pump screen and hear alarms? Many pumps have bright screens, large fonts, and vibration alerts.
- Caregiver Involvement: A committed caregiver who is willing to learn the technology is crucial for patients who need assistance.
- Realistic Goals: Work with your doctor to set clear goals, whether it's fewer injections, better overnight control, or more flexibility.
The Power of CGM Integration
Modern pump therapy is most powerful when paired with a Continuous Glucose Monitoring (CGM) system. This technology creates a life-changing partnership for many users.

A CGM sensor on your body checks your glucose every few minutes and sends the data to your pump. This enables powerful features:
- Hybrid Closed-Loop Systems: Often called "artificial pancreas" systems, these use CGM data to automatically adjust your background insulin 24/7. They can even give small correction doses, helping older adults achieve 75% time in a healthy glucose range.
- Predictive Low-Glucose Suspend: This critical safety feature automatically stops insulin delivery if it predicts your blood sugar is dropping too low, helping to prevent hypoglycemia. This provides tremendous peace of mind, especially for those living alone.
This integration transforms diabetes management from constant work to an informed partnership with technology, making an insulin pump for elderly patients a safer and more manageable option.
Navigating Costs, Coverage, and Safety
Understanding the financial and safety aspects is a critical step in the journey toward pump therapy.
Understanding Medicare Coverage for Insulin Pumps
A common question is whether insurance will cover an insulin pump for elderly patients. The good news is that Medicare Part B generally covers insulin pumps and supplies as Durable Medical Equipment (DME) for people with Type 1 diabetes.
However, there are key details to know:
- Quarterly Doctor Visits: To continue receiving supplies, Medicare requires a face-to-face visit with your doctor every three months. This is a valuable check-in to review your data and settings.
- Supply Challenges: Despite coverage, research shows over half of older pump users have faced supply delays, leading to dangerous practices like reusing supplies. Working with a reliable DME supplier is crucial to avoid these gaps.
- Out-of-Pocket Costs: You will likely be responsible for your Part B deductible and a 20% coinsurance.
At ProMed DME, we work with most insurance plans, including Medicare, to help you understand your benefits, minimize costs, and ensure you get your supplies on time. Our team includes a dedicated nurse to support you through the process.
Safety Precautions for the elderly using an insulin pump
With proper precautions, using an insulin pump for elderly patients is very safe. These habits are key to getting the benefits while minimizing risks:
- Skin Care: Change your infusion site every 2-3 days and rotate locations (abdomen, arms, thighs) to prevent irritation and infection.
- Preventing DKA: Pumps only use rapid-acting insulin. If delivery is interrupted, DKA can occur quickly. Be alert for signs of persistent high blood sugar and always have a backup plan with long-acting insulin and syringes.
- Hypoglycemia Preparedness: Even with a pump, lows can happen. Always carry fast-acting glucose. A CGM provides a huge safety advantage by giving early warnings.
- Caregiver Training: It's essential for a caregiver to be trained on how to use the pump, troubleshoot issues, and handle emergencies. Remote monitoring via CGM apps can provide extra peace of mind.
- Regular Follow-Ups: Consistent check-ins with your healthcare team are crucial for reviewing data, adjusting settings, and ensuring safe and effective pump use.
More on the benefits and challenges of diabetes technology highlights that ongoing partnership between the patient, caregivers, and healthcare team is essential for success.
Frequently Asked Questions about Insulin Pumps for Seniors
Here are answers to some common questions from older adults and their families.
Can someone with memory issues or dementia use an insulin pump?
It's possible, but only with a dedicated and fully trained caregiver who takes primary responsibility for managing the pump. This includes changing sites, programming doses, and responding to alarms. Without this level of support, it is not safe.
Automated systems with CGM integration can help by reducing the decision-making burden. Remote monitoring apps also allow caregivers to track glucose levels from afar. A thorough evaluation by the healthcare team of both the patient and the caregiver is essential to determine if a pump is a safe option. In cases of significant cognitive impairment, injections may remain the safer choice.
What kind of training is required to start on an insulin pump?
Comprehensive training is required and is usually provided by a certified pump trainer through your endocrinologist's office. The hands-on training covers:
- Basic pump operation, including menus and alarms.
- How to insert and change infusion sets or pods.
- How to calculate and deliver insulin for meals and corrections.
- Troubleshooting common issues.
- Creating and using a backup plan in case of pump failure.
Caregivers must attend and complete the same training. At ProMed DME, our on-staff nurse can also provide ongoing support as you adjust to pump therapy.
How does an insulin pump feel to wear every day?
While it's a common concern, most users report that after a few weeks, they barely notice their pump. Modern devices are small, lightweight, and designed for comfort and discretion.
- Daily Wear: Tubed pumps can be clipped to a waistband or kept in a pocket, while tubeless patch pumps stick directly to the skin under clothing.
- Sleeping: Sleeping with a pump is rarely an issue. You'll quickly find a comfortable position, whether the pump is next to you in bed or attached to your pajamas.
- Water Activities: This depends on the model. Many patch pumps are fully waterproof for showering and swimming. Some tubed pumps are water-resistant or can be temporarily disconnected.
The goal is for the pump to blend into your life. As one user said, "It just made my life easier... It makes a difference, especially on the golf course."
Conclusion
Choosing an insulin pump for elderly patients is a significant decision, but one with transformative potential. Modern pumps offer remarkable benefits, including better blood sugar control, fewer dangerous lows, and greater lifestyle freedom. Research confirms that older adults can achieve excellent results, often matching those of younger users.
However, pumps are not a one-size-fits-all solution. Success depends on a patient's motivation and physical and cognitive abilities. The technology can have a learning curve, and challenges are real. This is why a strong support system is non-negotiable. A team approach—involving the patient, dedicated caregivers, a thorough healthcare team, and a reliable medical supply company—makes all the difference.
Insulin pumps, especially when integrated with Continuous Glucose Monitoring (CGM), can be powerful tools for the right senior. The decision requires honest conversations about goals, abilities, and expectations.
At ProMed DME, we are part of that support team. We provide top-quality diabetes supplies, work with most insurance plans to minimize your costs, and have a dedicated nurse on staff to guide you. We're committed to helping you steer your journey toward better health.
The best diabetes management approach is the one that fits your life. Ready to explore your options? Contact us for your diabetes supply needs - we're here to help you figure out what works best for you.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



