Expecting and Pumping: Insulin Pump Therapy During Pregnancy

Navigating Type 1 Diabetes During Pregnancy
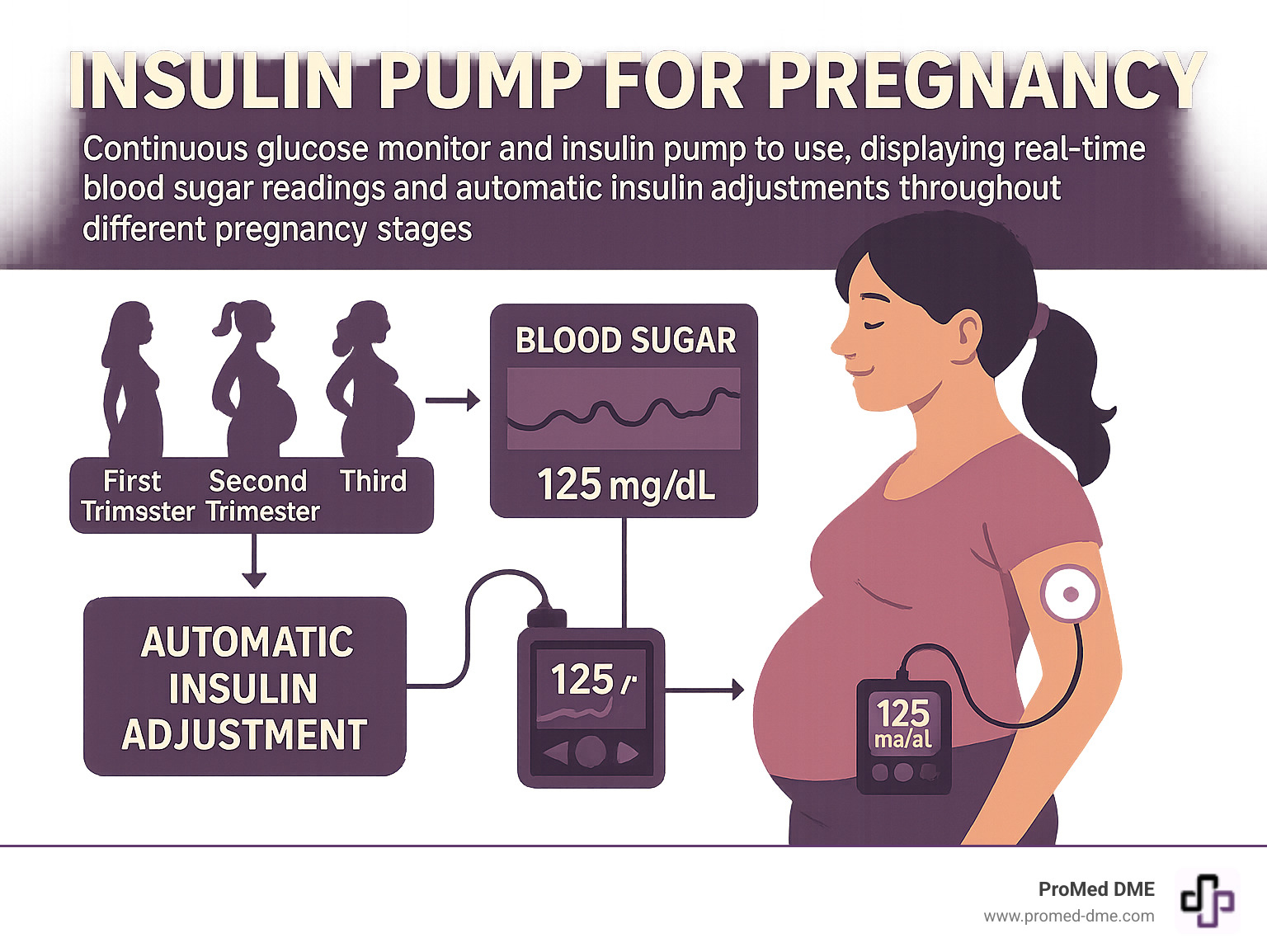
An insulin pump for pregnancy is a life-changing technology for expectant mothers with type 1 diabetes. During pregnancy, tight blood sugar control is critical for the health of both mother and baby.
Quick Answer for Insulin Pumps During Pregnancy:
- Safety: Insulin pumps are safe and increasingly recommended during pregnancy.
- Benefits: They offer better blood sugar control, reduced hypoglycemia, and lifestyle flexibility.
- Effectiveness: Closed-loop systems achieve 68% time in target range vs. 56% with standard care.
- Support: Proper use requires training and healthcare team coordination.
- Outcomes: Pump use may reduce pregnancy complications and improve neonatal health.
Managing type 1 diabetes during pregnancy presents unique challenges. Despite advances in care, half of babies born to women with type 1 diabetes still face complications like early birth and large birthweight.
The stakes are high, but modern technology offers hope. Insulin pumps, especially closed-loop systems, are improving outcomes by working 24/7 to maintain the tight blood sugar ranges pregnancy demands.
Pregnancy hormones make blood sugar control difficult, with insulin needs often doubling or tripling. Traditional injections struggle to keep up with these rapid changes.
This is where insulin pump technology shines. Unlike multiple daily injections, pumps adjust insulin delivery minute-by-minute, mimicking a healthy pancreas.
Quick insulin pump for pregnancy definitions:
- aace guidelines for insulin pump therapy
- advantages and disadvantages of insulin pump therapy
- continuous glucose monitoring system
The Unique Demands of Managing Diabetes During Pregnancy
Managing type 1 diabetes during pregnancy is a challenge. Your body changes the rules of diabetes management just as you're juggling the other excitements and worries of expecting a child.
Hormonal changes during pregnancy dramatically affect blood sugar. Starting around 16-20 weeks, these hormones create increased insulin resistance. It's not uncommon for your total daily insulin dose to double or even triple by your third trimester.
Fluctuating blood glucose levels can feel like trying to hit a moving target. This unpredictability is stressful when you know that tight control is crucial for your baby's health.
Morning sickness further complicates diabetes management. It's hard to calculate insulin for a meal you might not keep down, which can turn your carefully planned insulin schedule upside down.
The risk of complications makes this feel high-stakes. Blood sugar targets during pregnancy are much tighter to avoid problems like birth defects and large birth weight. At the same time, low blood sugar episodes become more dangerous; about 10% of pregnant women with diabetes are hospitalized at least once for severe hypoglycemia.
Despite incredible advances in diabetes care, the high stakes of T1D in pregnancy30406-X) remain real. Maternal and neonatal outcomes still show higher rates of complications compared to pregnancies without diabetes. This reality underscores why finding the right management approach is so critical.
Insulin Pump Therapy vs. Multiple Daily Injections (MDI)
For decades, multiple daily injections (MDI) were the standard, often requiring 7-10 shots a day. While MDI can work, it often lacks the precision needed for pregnancy's demands.
An insulin pump for pregnancy offers a different approach. It acts like a tiny, smart assistant, continuously delivering rapid-acting insulin through a small catheter under your skin, mimicking the pancreas much more closely than injections.
| Feature | Insulin Pump Therapy | Multiple Daily Injections (MDI) |
|---|---|---|
| Flexibility | High adjustable basal rates, precise bolusing, easy to adapt to changing needs (morning sickness, exercise) | Moderate requires careful timing of injections, less adaptable to spontaneous changes |
| Precision | Very high delivers insulin in small, precise increments (up to a tenth of a unit) | Moderate limited by the increments of insulin pens/syringes |
| Management | Continuous delivery, requires programming and site changes, integrates with CGM for advanced systems | Manual injections, requires multiple daily decisions, less real-time adjustment |
| Lifestyle | Greater flexibility for meal schedules, travel, and activity; discreet | Can be less discreet, may feel more restrictive for spontaneous activities |
The lifestyle flexibility of pumps is invaluable when pregnancy disrupts your routine. A pump can handle cravings or skipped meals with quick adjustments impossible with injection schedules.
Recent observational studies show lower blood glucose levels with pump therapy compared to MDI, especially in the first and second trimesters. The precision of pumps makes them well-suited for pregnancy. Many women also find postpartum insulin use easier to manage with a pump.
Key Benefits of Using an Insulin Pump for Pregnancy
The advantages of an insulin pump for pregnancy can transform your diabetes management during this crucial time.
Improved HbA1c levels are often a primary benefit. The consistent, precise insulin delivery helps achieve better average blood sugar, which reduces the risk of complications.
Reduction in hypoglycemia is a major improvement. Pumps can adjust or suspend insulin when glucose is trending low, making scary overnight lows less frequent.
Reduced glucose fluctuations mean fewer blood sugar roller coasters. The stable, adaptable insulin delivery smooths out highs and lows, which is crucial for healthy fetal development.
Greater lifestyle flexibility is where pumps shine. You can easily adjust for morning sickness or pregnancy cravings without disrupting your entire insulin schedule.
Easier management of morning sickness is a game-changer. You can eat what you can manage and bolus precisely for that amount.
Improved quality of life is the result of all these benefits. The mental burden of diabetes decreases when you have a tool that adapts to your needs, allowing you to focus more on enjoying your pregnancy.

This improvement in time-in-range represents hours each day where you and your baby are in the optimal zone for healthy development. Every percentage point improvement can make a meaningful difference.
The Rise of Closed-Loop Systems: A Game-Changer for Pregnancy
Imagine an insulin pump that adjusts itself. That's a closed-loop system, and it's revolutionizing how we approach insulin pump for pregnancy management.
What are closed-loop systems? Think of them as a personal diabetes assistant that never sleeps. These systems combine an insulin pump, a continuous glucose monitor (CGM), and a smart algorithm that connects them.
The CGM reads your blood sugar every few minutes and sends that data to the algorithm. The algorithm then tells your pump how much insulin to deliver—increasing it for highs and decreasing or stopping it for lows.
Automated insulin delivery takes much of the guesswork out of diabetes decisions. While you still need to bolus for meals, the system handles the constant background adjustments that pregnancy demands, 24/7.
The latest research on automated insulin delivery shows remarkable, game-changing improvements for pregnant women with type 1 diabetes.
Increased time in target range is where these systems excel. During pregnancy, blood sugar targets are much tighter, and automated systems are designed for this kind of precision.
A closed-loop system adapts instantly to pregnancy's unpredictable demands, adjusting your insulin minute by minute without you having to think about it.
How Closed-Loop Systems Improve Glycemic Control
Recent clinical trials show amazing results. Women using closed-loop systems during pregnancy spent 68% of their time in the ideal blood sugar range, compared to just 56% for those using standard insulin therapy. This translates to 2.5 more hours every single day with optimal blood sugars.
That extra time means a better environment for your baby's development and less fatigue and anxiety for you. Over an entire pregnancy, those hours add up to weeks of better control.
More time in target range is not just a statistic. Previous research on time in range and outcomes shows that even a 5% improvement leads to better pregnancy outcomes. Closed-loop systems deliver over a 10% improvement.
Less time in hyperglycemia was another key result. The closed-loop group spent only 29% of their time with high blood sugars, versus 41% for the standard care group. This is important, as high blood sugar can lead to complications.
Better overnight control is a life-changing benefit. The closed-loop group had significantly better overnight glucose control, allowing for more restful sleep without worry.
Lower HbA1c levels rounded out the results, with the closed-loop group achieving a meaningful average improvement of 0.31 percentage points.
These improvements happen because the system responds to changes faster than a person can manually, preventing highs and lows before they become serious.
Safety and Outcomes with Closed-Loop Technology
When you're pregnant, safety is a top concern. The good news is that closed-loop systems have proven to be remarkably safe during pregnancy.
Studies found similar rates of severe hypoglycemia and DKA (diabetic ketoacidosis) between closed-loop users and those on standard therapy, and the rates were very low in both groups. This confirms the technology doesn't increase risks.
An unexpected benefit was fewer unscheduled clinic visits. The closed-loop group had fewer crisis situations requiring immediate medical attention.
While the study wasn't large enough to prove better birth outcomes, the trends were encouraging. The significant improvement in blood sugar control strongly suggests potential for improved neonatal outcomes.
The 96% adherence rate speaks to how user-friendly these systems are. Women used them consistently through delivery, showing the technology makes management easier.
NICE recommendations for closed-loop systems now include their use for pregnant women with type 1 diabetes, reflecting growing confidence in their safety and effectiveness.

This represents the ultimate goal: healthy outcomes for both mother and child, supported by advanced diabetes technology.
Practical Guide to Using an Insulin Pump for Pregnancy
Switching to an insulin pump for pregnancy can feel overwhelming, but with the right preparation and support, it's an empowering decision for your health and your baby's.
Ideally, you should start pump therapy before you're pregnant. Achieving excellent blood sugar control (an HbA1c under 6%) for at least six months before conception gives you and your baby the best possible head start.
Working with your healthcare team is more important than ever. Expect frequent appointments with your endocrinologist, diabetes educator, dietitian, and obstetrician. Each team member provides unique expertise to help you steer the changing landscape of pregnancy with diabetes.
Education and training are the foundation of successful pump use. You'll learn everything from basics like changing infusion sites to advanced skills like interpreting CGM data. While it may seem like a lot at first, most people find it becomes second nature within a few weeks.
Insurance and access are common concerns. Most insurance plans cover insulin pump therapy during pregnancy. At ProMed DME, we work with most insurance plans and offer free shipping to help minimize your out-of-pocket expenses, so you can focus on your health.
Ongoing support is crucial as your body changes. You'll need regular check-ins with your team to review data and adjust settings. Most pump manufacturers also offer 24-hour support lines, which can be a lifesaver.
Mitigating Risks and Common Concerns
While insulin pumps are safe, being prepared for potential challenges is key.
Infusion site management is vital. Rotate your sites every 24-48 hours to prevent infections, irritation, and lumps that can interfere with insulin absorption. Using a calendar can help you keep track.
Preventing Diabetic Ketoacidosis (DKA) is even more critical during pregnancy. Because pumps use only rapid-acting insulin, any interruption in delivery can lead to DKA quickly. Stay vigilant, check your blood sugar and ketones if you feel unwell, and always have backup supplies.
Managing hypoglycemia remains important. You'll learn to recognize your body's changing patterns and adjust pump settings. Be alert, as hypoglycemia symptoms can change during pregnancy.
Having a backup plan provides peace of mind. Keep insulin pens on hand, know how to calculate doses manually, and have your team's emergency contact info accessible.
Most pump manufacturers offer 24-hour support to help with technical issues and arrange emergency replacements if needed. This support is invaluable during pregnancy.
Key Considerations for Using an Insulin Pump for Pregnancy
Successfully using an insulin pump for pregnancy means understanding that your settings will change frequently.
Choosing the right device involves working with your healthcare team to find a pump that fits your needs. The important thing is finding a device you feel confident using.
Understanding pump settings like basal rates, insulin-to-carb ratios, and correction factors is essential. Your team will help you master these concepts.
Adjusting for hormonal shifts is a regular part of your routine. Your insulin needs may decrease in early pregnancy, then increase dramatically later. Your team will guide you through these adjustments.
Labor and delivery planning should happen well before your due date. Discuss with your team whether to continue using your pump or switch to an IV. Many hospitals are comfortable with women keeping their pumps.
Postpartum adjustments are immediate. Your insulin needs will drop dramatically right after birth. If you breastfeed, your needs may be even lower. Your team will help you steer this rapid transition safely.
Frequently Asked Questions about Insulin Pumps and Pregnancy
It's natural to have questions when considering an insulin pump for pregnancy. Here are answers to the most common concerns.
Is it safe to use an insulin pump during pregnancy?
Yes, using an insulin pump for pregnancy is not only safe but increasingly recommended. It works 24/7 to provide the steady, adaptable insulin delivery your body needs.
Clinical trials show no unexpected safety issues compared to injections. In fact, research shows pumps help reduce the dangerous blood sugar swings that can harm you and your baby.
The importance of proper training is critical. You need to understand how your pump works and how to troubleshoot problems. Your healthcare team will ensure you're confident before you start.
Your healthcare team's role is your safety net. Through regular monitoring and adjustments, they help you steer the changes of pregnancy and keep your pump settings optimized.
While any medical device has minor risks, like infusion site issues, these are manageable with education. The benefits of better blood sugar control far outweigh these concerns.
Can I start using an insulin pump if I'm already pregnant?
Absolutely. While starting before pregnancy is ideal, many women successfully begin using pumps after they've conceived. The key is starting as early as possible to maximize the benefits.
Working with experienced endocrinologists is important in this case. Your doctor will move quickly to get you trained and comfortable. The benefits of improved glucose control can appear within days or weeks.
The training process may feel intensive, but you're learning skills that will benefit you for years. You'll master programming, bolusing, and interpreting CGM data.
A supportive diabetes care team makes all the difference. They will provide the intensive support and frequent monitoring you need during this transition.
How do I manage my insulin pump during labor and delivery?
Planning for labor and delivery with your insulin pump for pregnancy should be part of your birth plan discussions. Hospital protocols vary, so early communication with your diabetes team and obstetrician is essential.
Hospital protocols aim to keep blood glucose very stable, usually between 72-126 mg/dL (4.0-7.0 mmol/L). Some hospitals may prefer an IV insulin drip, while others are fine with you managing your pump.
Clear communication with your medical staff is vital. Ensure your nurses understand your pump and have contact info for your diabetes team. Bring written instructions for your settings.
Adjusting your basal rates is common during labor, often requiring significant reductions (50% or more). Your team will guide you based on your readings.
Continuous glucose monitoring during labor is incredibly valuable, providing real-time data for quick adjustments.
Post-delivery insulin needs change almost instantly. Your requirements often plummet to pre-pregnancy levels or lower within hours of birth. Your pump will need immediate reprogramming to prevent dangerous lows.
Your Partner in a Healthy Pregnancy Journey
Managing type 1 diabetes during pregnancy is challenging, but with the right technology and support, you can steer this journey with confidence.
The research is clear: insulin pump for pregnancy technology, especially closed-loop systems, is a game-changer. Spending 2.5 more hours per day in your target glucose range gives your baby the healthiest possible start.
This technology empowers mothers, offering peace of mind and a level of freedom unimaginable for previous generations. It allows you to sleep better and handle morning sickness without the constant worry of blood sugar swings.
However, technology is only part of the equation. Quality supplies and reliable support are crucial. Timely deliveries, smooth insurance processing, and expert guidance allow you to focus on what really matters—your growing family.
At ProMed DME, we understand the unique challenges of pregnancy with diabetes. Our approach is built around making your life easier. Our dedicated nurse is available to answer your questions, and we work with most insurance plans to minimize your out-of-pocket costs and stress.
With free shipping across the United States from our Stuart, Florida location, you'll have reliable access to the critical supplies you and your baby depend on.
Every expectant mother deserves to feel supported. We're here to handle the logistics so you can focus on the miracle of your pregnancy. Whether you're new to pump therapy or a seasoned user, we are committed to being your reliable partner.
Learn more about our diabetes supplies and support and find how we can help make your pregnancy journey smoother and more confident.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



