Navigating Medicaid for CPAP Supplies: A Breath of Fresh Air

Understanding Medicaid Coverage for CPAP Supplies
Does medicaid cover cpap supplies? Yes, Medicaid generally covers CPAP machines and essential supplies for beneficiaries diagnosed with obstructive sleep apnea (OSA), but coverage varies by state and requires meeting specific medical necessity criteria.
Quick Answer: What You Need to Know
- Coverage includes: CPAP machines, masks, tubing, filters, and humidifier chambers
- Requirements: Physician prescription, sleep study diagnosis, and proof of adherence (typically 4+ hours/night for 70% of nights)
- Initial period: 12-week trial period to demonstrate compliance
- State variation: Coverage details differ by state since Medicaid is state-administered
- Continued coverage: Dependent on consistent machine use and symptom improvement
If you've been diagnosed with sleep apnea, you know how life-changing CPAP therapy can be. You also know the equipment isn't cheap. The good news? Medicaid typically covers CPAP machines and supplies when medically necessary.
The challenge? Navigating the requirements, understanding what's covered, and proving you need the equipment. In April 2023, Medicaid covered 94 million Americans, many of whom struggle with sleep apnea. Yet the coverage rules can feel like a maze of documentation, trial periods, and state-specific requirements.
This guide breaks down exactly how to get your CPAP supplies covered by Medicaid. We'll walk through the diagnosis process, adherence requirements, finding suppliers, and understanding costs. Whether you're newly diagnosed or struggling to get your supplies covered, this article will help you steer the system.
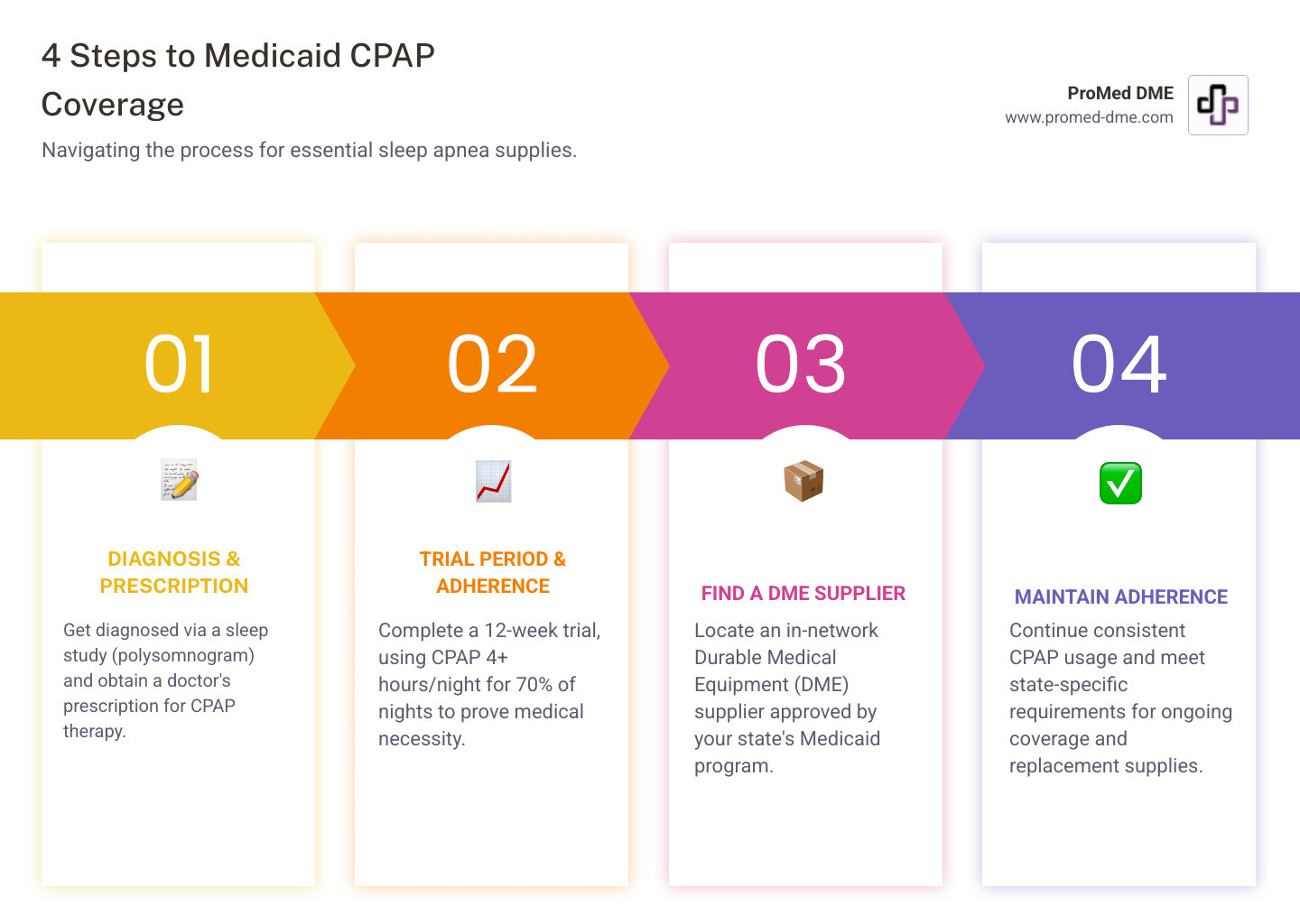
The Step-by-Step Process to Get Your CPAP Supplies Through Medicaid
Getting your CPAP equipment covered through Medicaid is manageable when you follow a few clear steps.

Step 1: Getting a Diagnosis and Proving Medical Necessity
Start with a face-to-face visit and be candid about symptoms like loud snoring, daytime sleepiness, or nighttime gasping. If OSA is suspected, your provider orders a sleep study (polysomnogram), typically within six months of the visit. The study (lab or home) measures breathing patterns and yields an AHI. Many states require an AHI of 15+ for coverage, or 5–14 with qualifying symptoms (for example, hypertension). Once diagnosed, your doctor writes a prescription for CPAP therapy. Keep the prescription, sleep study, and related medical records—these documents establish medical necessity for Medicaid.
Step 2: The Initial Trial Period and Adherence Rules
Most programs require a 12-week trial before long-term coverage. During this period, you must use the machine at least 4 hours per night on 70% of nights. CPAP devices record usage, so your DME supplier and provider can verify adherence. A follow-up visit confirms use and symptom improvement; coverage generally continues if you meet these criteria.
Step 3: Finding a Supplier and Getting Your Equipment
Work with a DME supplier enrolled with your state’s Medicaid program—ideally in-network. At ProMed DME, we work with most insurance plans, including Medicaid, and handle paperwork to minimize your out-of-pocket costs. We’re based in Stuart, Florida, and ship across the United States with free shipping.
Many states use a rent-to-own model (often 10–13 months). Continued rental payments depend on ongoing adherence. Beyond the CPAP machine, you’ll need essentials such as a mask (nasal pillows, nasal, or full face), tubing (heated or standard), filters, and a humidifier chamber. Replacement schedules vary by state and by item.
For broader context on CPAP therapy and insurance, see A guide to CPAP therapy from the Sleep Foundation.
A knowledgeable supplier makes a big difference. With a dedicated nurse on staff and responsive customer service, we help you get set up and stay covered.
Does Medicaid Cover CPAP Supplies in Every State?
Navigating does medicaid cover cpap supplies can be complicated because while Medicaid generally covers CPAP equipment, the specifics vary significantly depending on where you live.
Medicaid is a federal-state partnership. The federal government sets broad guidelines, but each state administers its own program. This means coverage rules, eligibility, and benefits vary significantly. What's covered easily in one state might require extra paperwork or have different replacement schedules in another.
So what exactly varies from state to state? Several important aspects of CPAP coverage can differ. Prior authorization is one big area where states diverge. Many states require your doctor and DME supplier to get approval from Medicaid before you receive your equipment. This isn't just a rubber stamp process – it involves submitting detailed medical records, sleep study results, and documentation proving why you need CPAP therapy. Some states make this process relatively straightforward, while others have more stringent requirements and longer wait times.
Replacement schedules for CPAP supplies also vary by state. Your mask cushions, filters, and tubing don't last forever – they need regular replacement to stay hygienic and effective. But how often Medicaid will cover these replacements is determined by your state's policy. One state might allow mask cushion replacements every month, while another might only cover them quarterly. As one industry source candidly notes, "You can probably bank on Medicaid covering your CPAP machine, but masks and supplies may be another story."
The question of whether your CPAP is a rental or a purchase can also have state-specific nuances. While many states follow a rent-to-own model (typically 10 to 13 months of rental payments before you own the machine), the exact duration can differ. Some states might also handle certain types of equipment differently. For example, Ohio Medicaid specifies that standard CPAP and BiPAP machines are a 10-month rent-to-purchase, but certain specialty BiPAP machines remain continuous rentals and never become the patient's property.
Specific supply coverage is another area where you might see differences. While the main CPAP machine is generally covered across all states, the accessories and supplies can be more variable. Some states might be more generous with covering different mask styles, heated tubing, or replacement filters, while others stick to covering only the absolute basics.
Some states also have special provisions that can work in your favor. North Carolina, for instance, has EPSDT (Early and Periodic Screening, Diagnostic, and Treatment), a federal Medicaid requirement that mandates coverage for medically necessary services for beneficiaries under 21. This can potentially allow for exceptions to standard policy limitations. Minnesota's Health Care Programs outline specific rules designating CPAP and BiPAP equipment as "capped rental only unless a primary payer requires purchase and authorization is obtained."
The bottom line? Because of these state-specific rules and coverage variations, you really need to check with your own state's Medicaid program to understand exactly what's covered in your area. Don't assume that what worked for your friend in another state will work the same way for you.
We know this can feel overwhelming, but you're not alone in figuring it out. You can find your state's Medicaid agency through this helpful resource. Your state agency will have the most current and accurate information about CPAP coverage in your specific location. And remember, your DME supplier should also be well-versed in your state's particular Medicaid policies and can help guide you through the process. At ProMed DME, we work with insurance plans across the country and understand how these state variations can impact your coverage – we're here to help make the process as smooth as possible.
Understanding the Costs: Medicaid, Medicare, and Out-of-Pocket Expenses
Let's talk money. Even with Medicaid coverage, it helps to understand what you might actually pay for your CPAP therapy. If you're eligible for both Medicare and Medicaid, or if you're wondering about potential surprise costs, this section will clear things up.
How does Medicaid cover CPAP supplies compared to Medicare?
First things first: Medicare and Medicaid are not the same thing. It's easy to mix them up because they both start with "Medi," but they serve different people and work in different ways. Medicare is primarily for folks aged 65 and older, or those with certain disabilities, regardless of how much money they make. Medicaid, on the other hand, is designed for people with lower incomes or disabilities, and the rules change depending on which state you live in.
Both programs generally cover CPAP machines and supplies when they're medically necessary, but they handle the costs differently. Medicare Part B covers durable medical equipment like CPAP machines after you've met your annual deductible. Once you've cleared that hurdle, Medicare pays 80% of the approved rental cost, leaving you responsible for a 20% coinsurance. Medicare typically uses a 13-month rental period, after which the machine becomes yours, though you'll still need to maintain consistent usage to keep getting supplies covered.
When we ask does medicaid cover cpap supplies, the answer depends on your state, as we've discussed throughout this guide. Generally speaking, if you meet your state's eligibility requirements and your doctor confirms the medical necessity, Medicaid covers the costs with little to no out-of-pocket expense. That's the beauty of Medicaid—it's designed to provide comprehensive coverage for people who need it most.
If you qualify for both programs (known as being dual-eligible), you have a strong safety net. Medicare acts as the primary payer, covering its 80% share first. Medicaid then acts as the secondary payer, often covering the remaining 20% coinsurance and your Medicare deductible. This coordination can dramatically reduce or eliminate your out-of-pocket costs.
What are potential out-of-pocket costs with Medicaid?
While Medicaid does an excellent job of minimizing costs, it's smart to know what expenses might still come your way. Nobody likes financial surprises, especially when you're just trying to get a good night's sleep.
Some states charge small copayments for certain services or prescriptions, though this is less common for durable medical equipment. It's usually just a few dollars if anything, but it's worth confirming with your state's program.
The bigger consideration is non-covered accessories. While your CPAP machine, mask, tubing, and filters are typically covered, some extras might not be. Those specialty CPAP pillows designed to work with your mask? The convenient cleaning wipes? Travel-specific accessories? These "convenience items" often aren't considered medically necessary, which means you'd pay for them yourself if you want them.
Here's the one that catches people off guard: adherence failure costs. Remember those usage requirements we talked about—4 hours per night for 70% of nights? If you don't meet them during your trial period or for continued coverage, Medicaid may stop paying the rental costs for your machine. At that point, you could become financially responsible for the equipment or need to return it. This is why we can't stress enough how important it is to stick with your therapy. It's not just about your health; it's about protecting your coverage.
Finally, state plan differences mean what's fully covered in one state might have limitations in another. Your neighbor across the state line might have slightly different coverage than you do. That's just the nature of a state-administered program. At ProMed DME, we work with most insurance plans and understand these variations, so we can help you steer what your specific Medicaid plan covers and minimize any out-of-pocket expenses.
Here's a quick comparison to help you see the differences at a glance:
| Feature | Medicaid | Medicare |
|---|---|---|
| Eligibility | Income-based, for low-income individuals/families, people with disabilities (varies by state) | Age 65+, or certain disabilities/conditions, regardless of income |
| Funding | Joint federal and state | Primarily federal |
| Coverage Scope | Varies significantly by state, generally comprehensive for medical necessity | National guidelines, covers medically necessary DME |
| Out-of-Pocket | Minimal to none (may cover Medicare deductibles/coinsurance for dual-eligibles) | 20% coinsurance after Part B deductible (if supplier accepts assignment) |
| Adherence Req. | Typically 4+ hours/night, 70% of nights (state-specific) | Typically 4+ hours/night, 70% of nights (national guidelines) |
| Primary Payer | Secondary payer if dual-eligible with Medicare | Primary payer if dual-eligible with Medicaid |
Understanding these details helps you plan ahead and avoid surprises. Our goal at ProMed DME is to make this process as smooth as possible, working with your insurance to keep your costs low so you can focus on what really matters—getting the restful sleep you deserve.
Frequently Asked Questions about Medicaid and CPAP Coverage
We know navigating insurance coverage can bring up a lot of questions. You're not alone in wondering about the details of does medicaid cover cpap supplies. Let's walk through some of the most common concerns we hear, so you can move forward with confidence.
Does Medicaid cover replacement CPAP supplies like masks and filters?
The short answer is yes – Medicaid typically covers replacement supplies like masks, tubing, filters, and headgear, but there's a bit more to the story. These supplies aren't just nice-to-haves; they're essential for effective and hygienic therapy. Think about it: a worn-out mask cushion can cause air leaks that make your therapy less effective, and old filters can't properly clean the air you're breathing all night.
The key thing to understand is that each state's Medicaid program operates on a set replacement schedule. This schedule is based on medical necessity and determines how often you can receive new supplies. For instance, you might be able to get a new mask cushion every couple of weeks, a full mask assembly every three months, tubing monthly or quarterly, and filters on a regular basis. These schedules exist to balance proper hygiene and therapy effectiveness with cost management.
What's covered as a replacement and how often can vary quite a bit depending on where you live. Your state determines the frequency, and sometimes the specific types of supplies covered. That's why it's so important to check with your DME supplier or contact your state's Medicaid office directly. They'll have the exact replacement schedule that applies to you, ensuring you get fresh supplies when you need them without any surprises.
What happens if I don't meet the CPAP usage requirements?
This is one of the most important questions, and we want to be completely honest with you. Your adherence to therapy – that 4 hours per night, 70% of nights requirement – isn't just a bureaucratic hoop to jump through. It directly determines whether Medicaid will continue covering your equipment.
If you consistently fall short of the usage requirements, especially during that crucial initial trial period, Medicaid may decide the therapy isn't working as intended. This can lead to coverage denial or discontinuation of your benefits. What does that mean in practical terms? You could become financially responsible for the CPAP machine if you're in a rent-to-own arrangement, or you might need to return the equipment to your supplier. It also means you're missing out on the health benefits that consistent CPAP use provides.
Adjusting to a CPAP machine can be challenging. If you're struggling with adherence due to discomfort or other issues, contact your doctor or DME supplier immediately. They can help with mask fitting, adjust pressure settings, or suggest different mask styles. Solving these problems is key to getting the restful sleep you need. Compliance not only keeps your coverage intact but, more importantly, keeps you healthy.
Does Medicaid cover BiPAP machines?
Yes, Medicaid does cover BiPAP machines, but with an important caveat: the criteria are usually stricter than for standard CPAP machines, and you'll almost always need prior authorization. BiPAP stands for Bi-level Positive Airway Pressure, and these machines deliver two different pressure levels – one for breathing in and a lower one for breathing out. This can make breathing feel much more natural and comfortable for certain patients.
BiPAP machines are typically prescribed when a standard CPAP isn't quite the right fit. Your doctor might recommend a BiPAP if you have complex sleep apnea that combines both obstructive and central components, if you've tried CPAP and it didn't work for you (what we call CPAP failure), or if you have other respiratory conditions like COPD or restrictive lung diseases that require more sophisticated breathing support.
Because BiPAP machines are more advanced and generally more expensive than CPAP devices, Medicaid wants thorough documentation showing why you need this higher level of therapy. Your doctor will need to provide detailed justification explaining why a BiPAP is medically necessary for your specific situation, often including documentation of a failed CPAP trial or specific diagnostic test results.
Just like with CPAP machines, coverage details for BiPAP vary by state. Some states cover them under a rent-to-purchase model, while others classify certain advanced BiPAP models as continuous rentals that never become your property. The bottom line? If your doctor recommends a BiPAP, work closely with them and your DME supplier to ensure all the necessary documentation is submitted for prior authorization. We're here to help steer that process and get you the equipment you need for better breathing and better sleep.
Your Path to Restful Sleep
Understanding does medicaid cover cpap supplies comes down to three pillars: get a documented diagnosis with a sleep study and prescription, meet adherence requirements (4 hours on 70% of nights), and follow your state’s rules for prior authorization and replacement schedules.
State policies differ, so confirm details with your Medicaid office or ask your DME supplier to verify specifics for you.
At ProMed DME, we simplify the process. We’re based in Stuart, Florida, ship quality durable medical supplies across the United States, and work with most insurance plans to minimize out-of-pocket expenses. You’ll get free shipping, guidance from our dedicated nurse, and help with documentation and adherence.
Get your covered medical supplies today and take the next step toward consistent, restorative sleep.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



