How to Find Medicare-Approved DME Without the Headache

Explaining Medicare-Approved DME
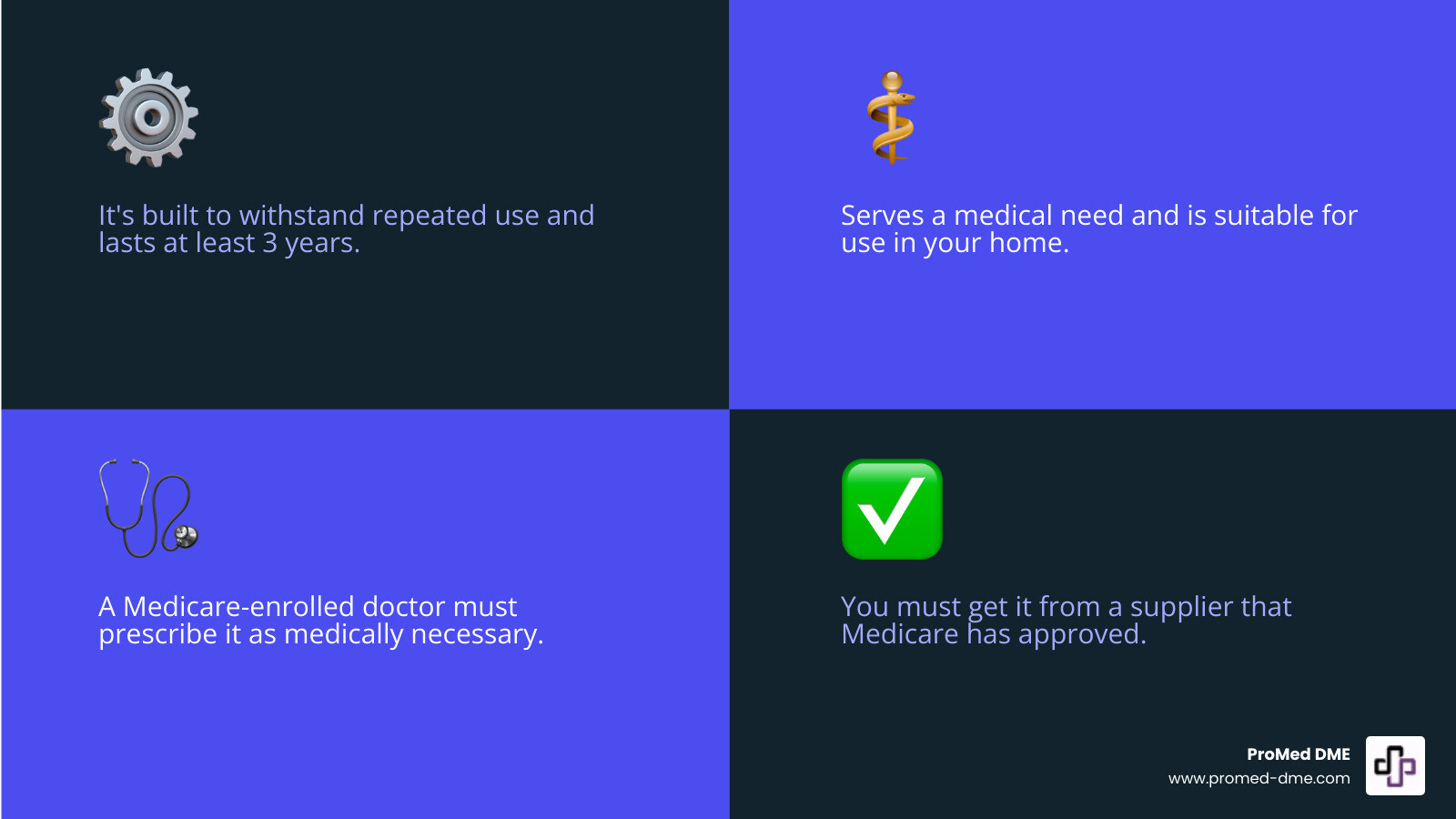
Finding medicare approved dme can feel like a maze, but understanding what Medicare covers is simpler than you think. For Durable Medical Equipment (DME) to be Medicare-approved, it must meet specific criteria.
Here are the key requirements for equipment to be considered Medicare-approved DME:
- Durable: It's built to withstand repeated use.
- Medical Purpose: It serves a medical need, not just comfort or convenience.
- Home Use: It's suitable for use in your home.
- Long-Lasting: It's expected to last for at least three years.
- Prescribed: A Medicare-enrolled doctor must prescribe it as medically necessary.
- Approved Supplier: You must get it from a supplier that Medicare has approved.
This guide will cover what DME is, how Medicare covers it, and how to find reliable suppliers, making it easier to access your essential medical equipment.
Medicare approved dme helpful reading:
What is Durable Medical Equipment (DME) According to Medicare?

Durable Medical Equipment (DME) isn't just any health item. Medicare specifically defines what counts as medicare approved dme to ensure it helps with a medical need and is built to last.
First, DME must be durable, meaning it can withstand repeated use. Examples include walkers and wheelchairs built for long-term use, not disposable items.
It must also serve a medical purpose, helping with a health condition, not just providing comfort. A CPAP machine for sleep apnea is a good example. The equipment is also generally not useful to someone who isn't sick or injured.
The equipment must be for use in the home. Medicare generally doesn't cover DME in a hospital or skilled nursing facility, as care is already provided there.
Finally, to be considered durable, the equipment must have an expected life of at least 3 years.
The "Medically Necessary" Standard
Beyond the DME definition, the equipment must be "medically necessary." This means a Medicare-approved doctor must prescribe it as a formal order. The prescription must state the equipment is for treating an illness or injury. For example, a walker for post-surgery recovery is medically necessary, while an adjustable bed for comfort is not. Medicare covers what's essential for your health. Understanding these medically necessary criteria is crucial for getting your equipment covered.
Understanding Your DME Coverage and Costs
Understanding how to pay for your medicare approved dme can be puzzling. Let's clarify how Medicare's different parts and other plans help cover the costs.
Most medicare approved dme falls under Medicare Part B (Medical Insurance). For those with Original Medicare, Part B covers outpatient services, doctor visits, and essential medical equipment.
Medicare Advantage Plans (Part C) must cover the same medicare approved dme as Original Medicare. However, they may have different rules, such as requiring in-network suppliers or prior authorization for certain items. Always check with your plan directly.
Medigap policies (Medicare Supplement Insurance) help lower out-of-pocket costs. They work with Original Medicare to pay for expenses like coinsurance and deductibles.
Costs with Original Medicare
With Original Medicare Part B, after you meet your yearly deductible, Medicare covers 80% of the cost for medicare approved dme. You are responsible for the remaining 20% coinsurance.
The Medicare Part B deductible for 2025 is $257. After you pay this amount for covered services in a year, Medicare begins paying its share.
For example, imagine you need a piece of DME that Medicare approves for $1,000, and you've already met your deductible for the year. Here's how that usually works out:
- Medicare pays a big chunk: $800 (that's 80% of $1,000).
- You pay the rest: $200 (that's your 20% coinsurance).
This 20% coinsurance applies to each item, so costs can add up if you need multiple pieces of equipment.
How Other Plans Affect Costs
Medicare Advantage and Medigap plans can significantly change your out-of-pocket costs for medicare approved dme.
Medicare Advantage Plans must cover the same medically necessary DME as Original Medicare but can have different cost-sharing rules, like fixed copayments instead of coinsurance. They have an annual out-of-pocket maximum but often require you to use in-network suppliers and get prior authorization for some items. Contact your plan to understand their specific rules and costs.
Medigap policies are designed to cover the 20% coinsurance that Original Medicare doesn't pay for your medicare approved dme. Depending on the plan, it could cover from 50% to 100% of your out-of-pocket costs for Part A and B services, including DME. This can significantly reduce your financial burden. It's wise to compare Medigap coverage policies.
To help you visualize the differences, here's a quick look at how your DME costs might stack up depending on your Medicare setup:
| Cost Aspect | Original Medicare (Part B) | Medicare Advantage Plan (Part C) | Medigap Policy (with Original Medicare) |
|---|---|---|---|
| Deductible | Yes (Part B deductible applies, $257 in 2025) | Varies by plan; may have its own deductible | Part B deductible still applies, but some plans may cover it |
| Coinsurance/Copay | 20% of Medicare-approved amount | Varies by plan; may be a copay per item or percentage coinsurance | 0% - 20% (Medigap covers most/all of the 20% coinsurance) |
| Supplier Network | Any Medicare-enrolled supplier | Typically requires in-network suppliers | Any Medicare-enrolled supplier |
| Prior Authorization | Generally not required by Original Medicare | Often required for certain high-cost DME | Generally not required (follows Original Medicare rules) |
| Out-of-Pocket Max | No annual limit | Yes, legally required | No annual limit (but significantly reduces out-of-pocket costs) |
| Overall Cost | Can be high if extensive DME is needed | Predictable annual costs due to out-of-pocket max, but network restrictions | Lowest out-of-pocket costs for covered DME, but requires separate premium |
A Guide to Medicare-Approved DME Items
Medicare approved dme includes more than just wheelchairs and walkers. Medicare covers a wide range of equipment, supplies, prosthetics, and orthotics to help you manage health conditions at home. The variety is remarkable, from blood sugar monitors for diabetes to CPAP machines for sleep apnea, reflecting the different tools needed for various health conditions.
Common Examples of Medicare-Approved DME
Commonly covered items include essentials for managing specific conditions.
For diabetes, blood sugar monitors and test strips, lancets, and other testing supplies are typically covered. For mobility, Medicare covers canes, walkers, crutches, wheelchairs, and scooters (manual and power) when medically necessary.
Hospital beds for home use often qualify for those recovering from surgery or managing a chronic condition. For respiratory conditions, covered items include CPAP devices for sleep apnea, nebulizers and their medications for asthma or COPD, and oxygen equipment and accessories.
Patient lifts for safe transfers and commode chairs for those confined to bed are also covered. Other covered items include infusion pumps and supplies, suction pumps, traction equipment, and pressure-reducing support surfaces.
Medicare also covers orthotics and prosthetic items like braces, artificial limbs, and therapeutic shoes for people with diabetes. All these items require a doctor's prescription and must be medically necessary.
What Equipment and Supplies Medicare Does Not Cover
Medicare draws a clear line between what's medically necessary and what's for convenience or comfort.
Convenience and comfort items are generally not covered. This includes air conditioners, grab bars, bathtub seats, stairway elevators, and massage devices.
Home modifications like ramps or widening doorways are not covered, as they are considered home improvements. Items designed only for use outside the home typically don't qualify as medicare approved dme due to the strict "home use" requirement.
Most disposable supplies like bandages or incontinence pads are not covered, unless they are part of a covered service or used with covered DME (e.g., test strips for a glucose monitor). Items not expected to last at least three years do not qualify as "durable."
Medicare focuses on medical necessity, not general quality of life. For a full list of exclusions, see this resource on equipment excluded from coverage.
Your Step-by-Step Process for Getting DME

Getting medicare approved dme is a clear process that begins with your doctor and involves teamwork between you, your doctor, and your supplier.
The first step is a doctor's prescription. A Medicare-approved provider must confirm the equipment is medically necessary, often requiring a face-to-face visit. Your medical records must clearly document the need for the specific DME for Medicare to approve coverage.
With a prescription, you'll find out if Medicare will rent or buy the equipment. Medicare often rents costly items like power wheelchairs. After a set number of rental payments (often 13 continuous months), ownership may transfer to you. Less expensive items may be purchased outright.
How to Find a Medicare-Approved DME Supplier
Finding the right supplier for your medicare approved dme is crucial. You must use a supplier that is enrolled with Medicare. Some are simply "Medicare-Enrolled," while others are "Medicare-Participating." Participating suppliers have an agreement to "accept assignment," meaning they accept the Medicare-approved amount as full payment.
A supplier that accepts assignment cannot charge you more than your 20% coinsurance and any unmet deductible. A non-participating supplier can charge more than the Medicare-approved amount, leaving you to pay "excess charges." Choosing a participating supplier is the best way to avoid extra costs.
Use Medicare's online supplier directory to find a supplier. Search by ZIP code and equipment type, then call to confirm they accept assignment for your specific DME.
Understanding Repairs, Replacements, and Maintenance
Medicare also has rules for repairs and maintenance of your medicare approved dme.
Responsibility for repairs depends on whether you rent or own the equipment:
- Rented Equipment: The supplier is usually responsible for maintenance and repairs.
- Owned Equipment: You are typically responsible for arranging maintenance and repairs. Medicare may still cover 80% of the approved cost.
Medicare defines a "reasonable useful lifetime" for DME, typically 5 years. If your equipment breaks before 5 years and can't be fixed, Medicare may cover a replacement if it's still medically necessary. After 5 years, Medicare may cover a new item if you still need it.
In emergencies like a natural disaster, Medicare may help cover replacement costs for lost or damaged equipment. If you have a Medicare Advantage Plan, contact them directly for their specific rules.
Staying Safe: How to Spot and Report DME Fraud
Medicare approved dme fraud is common, with scammers targeting beneficiaries. Knowing the signs can help protect you.
Unsolicited calls or visits offering "free" medical equipment are a major red flag. Legitimate suppliers do not cold-call or make uninvited house calls. Scammers may claim to be from Medicare or your doctor's office.
Aggressive marketing tactics, like high-pressure sales or limited-time offers, are another warning sign. Legitimate suppliers give you time to consider your options.
Offers of "free" equipment are usually a scam. You are typically responsible for a deductible and 20% coinsurance. Scammers offering free items often plan to bill Medicare for things you don't need or never receive.
Protect your Medicare number like a credit card. Only share it with your trusted healthcare providers and never give it to an unsolicited caller.
Review your Medicare Summary Notice (MSN) quarterly. Check for services or equipment you didn't receive or recognize and report any discrepancies.
If you suspect fraud, report it quickly. The Senior Medicare Patrol (SMP) is a free resource that helps beneficiaries detect, prevent, and report healthcare fraud.
Questioning unexpected offers and reviewing statements is smart, not paranoid. It protects you from fraud.
Frequently Asked Questions about Medicare and DME
Navigating medicare approved dme can be complex. Here are answers to some common questions.
Do I have to rent my DME, or can I buy it?
The answer depends on the item. Medicare often prefers to rent expensive DME, like power wheelchairs or hospital beds. Many items fall into a "capped rental" category, where Medicare makes rental payments for up to 13 continuous months, after which the supplier must transfer ownership to you. Less expensive items may be purchased from the start. Your medicare approved dme supplier can tell you if an item is for rental, capped rental, or purchase.
What's the difference between a Medicare-enrolled and a Medicare-participating supplier?
This distinction is important for your out-of-pocket costs. A Medicare-enrolled supplier has met Medicare's basic requirements to bill Medicare.
A Medicare-participating supplier goes a step further by signing an agreement to "accept assignment." This means they accept the Medicare-approved amount as full payment and cannot charge you more than your 20% coinsurance and any unmet deductible. A non-participating supplier has not signed this agreement and can charge more than the Medicare-approved amount, leaving you responsible for "excess charges." Choosing a participating supplier is the financially smarter choice for your medicare approved dme.
What should I do if my request for DME is denied?
A denial for medicare approved dme is not the final word. You have the right to appeal, and many denials are overturned.
First, review your Medicare Summary Notice (MSN) to understand the reason for the denial. Next, talk to your doctor. If the denial was for a lack of medical necessity, your doctor can provide additional documentation to support your case.
Then, begin the multi-step appeals process, starting with a "redetermination." For free, unbiased help, contact your local State Health Insurance Assistance Program (SHIP). They can guide you through the appeals process. Many denials are due to correctable administrative issues.
Conclusion
Navigating medicare approved dme is manageable. Understanding the rules and processes helps you access the equipment you need for a healthier, more independent life at home.
Key takeaways: start with a doctor's order establishing medical necessity, choose a Medicare-approved supplier that accepts assignment, and be aware of out-of-pocket costs. Being informed empowers you to make the best decisions for your health and finances.
For specialized supplies like urology, diabetes, wound care, or bracing products, working with an experienced provider is key. At ProMed DME, we are committed to delivering top-quality products with exceptional customer service. We offer free shipping across the United States, have a dedicated nurse on staff to answer your questions, and work with most insurance plans to minimize your out-of-pocket expenses. We're here to support you on your health journey, ensuring you get the medicare approved dme you need without the unnecessary stress.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.




