Is Your DME Covered? A Deep Dive into Blue Cross Blue Shield Policies

Why Understanding Blue Cross DME Coverage Matters
Understanding your Blue Cross DME coverage is crucial for getting the medical equipment you need without unexpected costs. Knowing what's covered for items like wheelchairs, oxygen equipment, or diabetic supplies can save you hundreds or thousands of dollars.
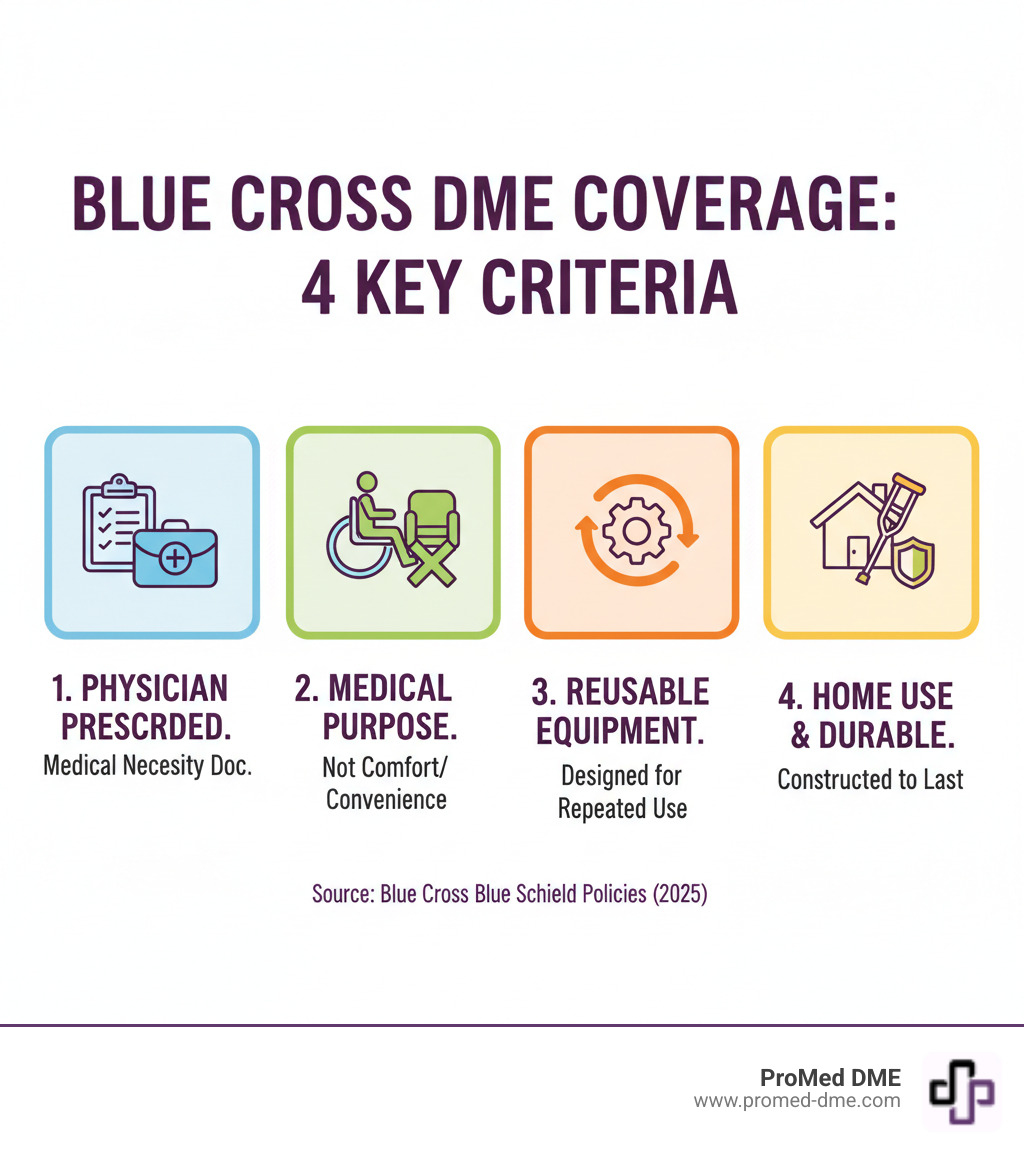
Quick Answer for Blue Cross DME Coverage:
- Medical Necessity Required: Equipment must be prescribed by your doctor for a medical condition.
- Home Use Only: DME must be appropriate for use in your home environment.
- Durable & Reusable: Equipment must last at least 3 years with repeated use.
- In-Network Savings: Using preferred DME providers reduces your out-of-pocket costs significantly.
Blue Cross Blue Shield plans cover basic durable medical equipment when it meets specific criteria. All Medicare Advantage plans cover essential equipment, and many will cover advanced equipment if your doctor says it’s medically necessary. Medicare Part B typically covers 80% of approved costs, leaving you responsible for the remaining 20% coinsurance.
Successful DME coverage depends on three factors: proper physician documentation, using approved suppliers, and knowing whether to rent or purchase. Your specific coverage depends on your plan type—whether you have Medicare Advantage, Medicare Supplement, or a commercial Blue Cross plan. Each has different rules for preferred providers, prior authorization, and cost-sharing.
Blue cross dme vocab explained:
Defining DME: What Blue Cross Considers Covered and Not Covered
Understanding what Blue Cross Blue Shield considers durable medical equipment can save you from surprise denials. It's not as simple as "if it's medical, it's covered"; a specific framework determines if your equipment qualifies.
Blue Cross DME must meet four essential criteria: it must serve a medical purpose, be necessary due to your medical condition, be prescribed by a physician, and be durable enough for repeated home use (typically lasting at least three years). For example, a prescribed hospital bed serves a clear medical purpose, while a standard comfortable mattress does not meet the medical necessity standard.
Your doctor's prescription is the foundation of your claim. Without proper documentation of medical necessity, even obviously medical equipment won't be covered. Single-use items or supplies that need frequent replacement fall into different coverage categories.

What Equipment is Covered?
When your equipment meets Blue Cross's criteria, you'll find coverage for a comprehensive range of items.
- Mobility equipment: Wheelchairs (manual and electric), walkers, canes, and crutches are essential tools that prevent falls and enable daily activities.
- Respiratory support: Oxygen concentrators, nebulizers, and CPAP or BiPAP machines for sleep apnea qualify when medically necessary.
- Complex medical equipment: Hospital beds, pressure mattresses, patient lifts, and ventilators are included when prescribed.
- Specialized monitoring equipment: Continuous glucose monitors, apnea monitors, and infusion pumps help manage chronic conditions from home.
- Other covered items: This includes kidney machines for home dialysis, bili blankets for infant jaundice, and traction equipment.
Every item must be medically necessary and prescribed by your doctor.
What Equipment is Not Covered?
Knowing what Blue Cross doesn't cover is equally important to avoid claim denials.
- Comfort and convenience items: A regular mattress or wheelchair cup holders are not considered medical equipment.
- Items with significant non-medical uses: Air conditioners, humidifiers, and air purifiers are generally not covered as they are used by healthy people too.
- Home and vehicle modifications: Stair lifts, ramps, and grab bars are considered environmental changes, not medical equipment.
- Exercise equipment: Items like treadmills or stationary bikes are generally excluded due to widespread non-medical use.
- Standard bathroom equipment: Shower chairs and raised toilet seats usually aren't covered, though some plans make exceptions for medical-grade commode chairs.
- Breast pumps: These have special rules that vary by plan, so always check your specific benefits.
In short, if equipment primarily serves comfort, convenience, or has major non-medical applications, Blue Cross typically won't cover it as DME. The focus is on true medical necessities.
Your Step-by-Step Guide to Obtaining Blue Cross DME
Getting your durable medical equipment is a straightforward process. This section walks you through the three key steps, from the doctor's visit to delivery.
Step 1: Get a Physician's Prescription and Documentation
Your doctor is your greatest ally for getting Blue Cross DME coverage approved. A simple prescription isn't enough; Blue Cross requires a full medical story. The documentation must be thorough and specific, identifying the exact equipment you need.
Medical necessity documentation is key. Your physician must explain in detail why the equipment is essential for managing your condition and why you can't function safely without it. This includes:
- A plan of treatment outlining how long you'll need the equipment and expected outcomes.
- Clinical and functional status documentation detailing your specific mobility limitations, risk of falls, or other medical conditions that make the DME necessary.
The more detailed this documentation, the stronger your case for coverage. For reference, you can see the level of detail insurers expect by reviewing examples like the Durable Medical Equipment (DME) Physician Order Forms. While this is a Texas Medicaid form, it shows the comprehensive information Blue Cross typically requires.

Step 2: Find an Approved In-Network DME Supplier
Your choice of supplier greatly affects your out-of-pocket costs. In-network suppliers are your best bet for maximizing coverage and minimizing costs, as they have contracts with Blue Cross to accept specific payment rates. Using them helps you avoid balance billing surprises.
Many Blue Cross plans also have preferred providers where you'll receive the highest level of benefits, often meaning lower copayments or coinsurance. Out-of-network suppliers may provide coverage at lower benefit levels, costing you substantially more.
To find an approved supplier, check your Blue Cross member portal online or call the customer service number on your ID card. Your doctor's office is another valuable resource, as they often work with reliable, in-network suppliers.
At ProMed DME, we work with most insurance plans and understand the ins and outs of Blue Cross DME benefits. We offer free shipping nationwide and have a dedicated nurse on staff to help you steer your coverage.

Step 3: Understand Billing and Coding for Blue Cross DME
Understanding DME billing basics can save you headaches and ensure claims process smoothly. Every piece of equipment has a unique HCPCS code that tells Blue Cross what you received.
In addition, modifiers (two-character codes) provide crucial details. For example, the RR modifier indicates rental, while the NU modifier means purchase. Using the wrong one can cause claim rejection or incorrect processing, affecting your long-term costs.
Some equipment has specific rules. For instance, breast pumps often default to purchase pricing, and certain oxygen accessories require the NU modifier. Specialized modifiers like AU (urological supplies) or AW (compression stockings) are also used.
Your DME supplier should handle this coding, but knowing the basics helps you ask the right questions. For technical details, providers reference policies like the DMEPOS Modifiers Policy.
Managing Costs: Patient Responsibilities and Medicare Coverage
Understanding your financial responsibility for Blue Cross DME is about planning for out-of-pocket costs and making smart decisions about your care.
Your Financial Share: Deductibles, Coinsurance, and Limits
Even with good insurance, you will likely share some of the cost for your DME. Here's what to expect:
- Deductibles: This is the amount you pay out-of-pocket before your Blue Cross plan begins to pay. Many plans apply this deductible to DME.
- Coinsurance: This is your share of the approved costs, usually a percentage (e.g., 20%). Using preferred providers often lowers your coinsurance rate.
- Copayments: Some plans use a flat dollar amount for certain DME items or supplies.
- Annual Limits: Be aware of annual limits on certain items, like speech-generating devices, which might be capped at a specific dollar amount per year. Anything beyond that limit is your responsibility.
To manage these costs, always check your specific plan's Summary of Benefits or call member services. Your exact financial responsibilities can vary significantly between Blue Cross plans.
Rent vs. Purchase: The Blue Cross Guidelines
Blue Cross has clear guidelines that often determine whether you rent or buy DME.
- Purchase: Inexpensive equipment (under $200) like canes and walkers is almost always purchased. Items that are routinely purchased, such as blood glucose monitors, also fall into this category.
- Rental: Rental is common for temporary needs (e.g., crutches after surgery) or for high-maintenance equipment like ventilators. For expensive equipment (over $200), Blue Cross may require a rental trial period to ensure it works for you before approving a purchase.
| When You'll Rent | When You'll Purchase |
|---|---|
| Short-term medical need (temporary injury) | Equipment costs under $200 |
| High-maintenance equipment requiring specialized service | Items routinely purchased (glucose monitors, braces) |
| Complex devices like ventilators | Long-term use expected based on your condition |
| Trial period to ensure proper fit and function | After successful rental trial period proves effectiveness |
When rental equipment reaches its maximum reimbursement, the rental company retains ownership, but you continue to use it as long as it's medically necessary.
How Medicare Works with Blue Cross DME
If you have both Medicare and Blue Cross, their interaction significantly impacts your Blue Cross DME costs.
- Medicare Part B: This is the foundation for most DME coverage. It typically covers 80% of approved costs after you meet your annual deductible, leaving you with 20% coinsurance.
- Medicare Advantage (Part C) plans: These all-in-one plans cover everything Original Medicare does, often with additional benefits. The key difference is the network requirement—you must use specific DME providers for the best benefits.
- Medicare Supplement (Medigap) plans: These work alongside Original Medicare to cover what Medicare doesn't, such as the 20% coinsurance and deductibles. This results in significantly lower out-of-pocket costs and more flexibility in choosing Medicare-approved suppliers.
Regardless of your plan, the core requirements remain: medical necessity, a doctor's prescription, and using an authorized supplier. ProMed DME works with most insurance plans, including Medicare, to minimize your expenses.
Frequently Asked Questions about Blue Cross DME Coverage
Here are answers to the most common concerns about Blue Cross DME coverage.
How are repairs, maintenance, and replacement of DME handled?
Blue Cross DME coverage typically helps with these costs, but the process differs depending on whether you rent or own the equipment.
- If you purchased your DME, Blue Cross usually covers necessary repairs, maintenance, and replacement for equipment that breaks down. Manufacturer warranties may also cover initial defects. Many suppliers offer covered maintenance agreements for ongoing care.
- If you're renting your DME, the monthly rental fee is all-inclusive. It covers maintenance, repairs, replacements, supplies, and accessories, as well as delivery and setup. You will not receive separate bills for these services.
However, if equipment is damaged due to misuse or neglect, you will likely be responsible for the repair or replacement costs.
What happens if my request for DME is denied?
A denial is not the final word; you have the right to appeal. Many denials are overturned with the right information.
First, read the denial letter carefully to understand the reason, which is often a lack of medical necessity, missing documentation, or using an out-of-network supplier.
If the issue is medical necessity, work with your doctor to provide more detailed medical records or test results. Then, follow the appeals process outlined in your denial letter, submitting a written request for review with the new documentation. Don't give up if the first appeal doesn't work, as there are often multiple levels of review.
Your Blue Cross member services team can guide you through this process. At ProMed DME, we also support customers through appeals, as our team understands what documentation insurers require.
Are breast pumps covered as DME?
Yes, most Blue Cross DME plans cover breast pumps, thanks to the Affordable Care Act. Most plans cover a double-electric breast pump as medically necessary, and claims typically default to purchase pricing.
However, specific coverage varies by plan. Some plans cover manual pumps, others only electric; some require a prescription, while others don't. The timing of when you can receive the pump can also differ.
Always check with your Blue Cross plan directly to understand your specific breast pump benefits, including what's covered, when you can get it, and which suppliers to use.
Conclusion
Getting the Blue Cross DME coverage you need doesn't have to feel like solving a puzzle blindfolded. Once you understand how the system works, you can confidently get the medical equipment that helps you live your best life.
The secret to success really comes down to three simple things. Medical necessity is everything - your doctor needs to clearly explain why you need specific equipment and provide detailed documentation that goes way beyond a quick note. Think of it as building your case with solid evidence.
Your choice of supplier makes a huge difference in your wallet. Using approved, in-network DME suppliers isn't just a suggestion - it's your ticket to the lowest possible costs. Out-of-network providers can leave you paying significantly more, sometimes the entire bill.
Every Blue Cross plan is unique, and yours has specific rules about deductibles, coinsurance, and whether renting or buying makes more sense. Whether you have a commercial plan, Medicare Advantage, or Medicare Supplement, taking a few minutes to understand your particular benefits can save you hundreds of dollars and prevent frustrating surprises.
We know that dealing with insurance paperwork while managing health challenges isn't anyone's idea of fun. That's exactly why ProMed DME exists - to make this process as smooth as possible for you. We work with most insurance plans and handle the complicated stuff so you don't have to. Our dedicated nurse is always available to answer your questions, explain your coverage, and make sure you get exactly what you need.
Free shipping across the United States means your supplies arrive at your door without extra costs. We believe exceptional customer service and top-quality products should be the standard, not the exception.
Ready to get the medical supplies you need without the headache? We're here to help every step of the way.
Get started with your DME needs

Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



