The Tell-Tale Signs of Low Blood Sugar

Why Recognizing the Signs of Low Blood Sugar Could Save Your Life
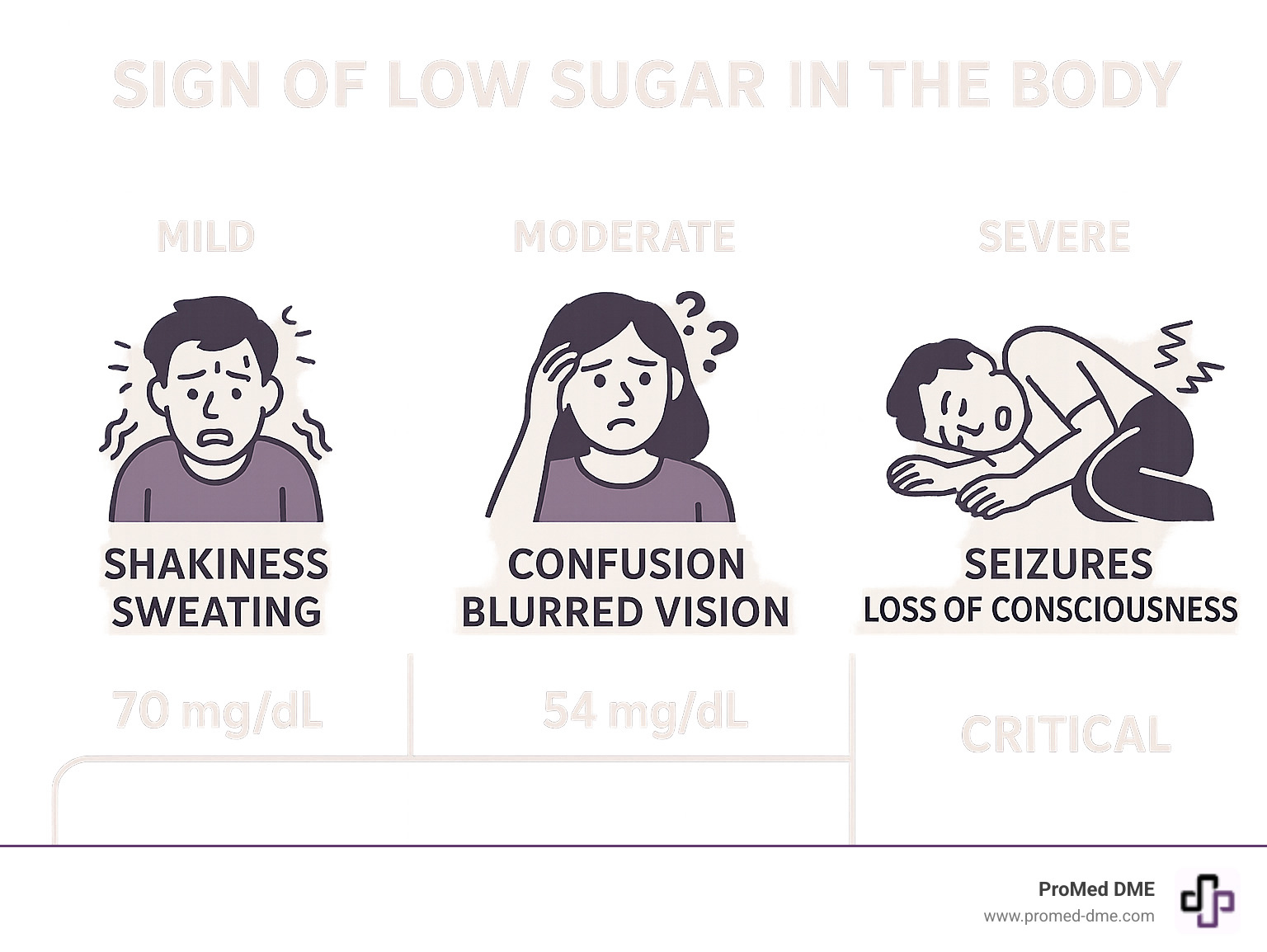
Sign of low sugar in the body can appear suddenly and progress rapidly from mild discomfort to a life-threatening emergency. Low blood sugar, medically known as hypoglycemia, occurs when glucose levels drop below what your brain needs to function properly.
Common signs of low blood sugar include:
- Shakiness and trembling
- Sweating and clamminess
- Fast heartbeat
- Anxiety and nervousness
- Hunger and nausea
- Dizziness and confusion
- Blurred vision
- Severe cases: seizures, loss of consciousness
Your brain depends entirely on glucose for energy. When blood sugar drops below 70 mg/dL for people with diabetes (or 55 mg/dL for those without), your body releases stress hormones like adrenaline. This creates the shakiness, sweating, and racing heart that serve as your body's alarm system.
The key is recognizing these warning signs early. As one medical expert notes: "When glucose levels approach severely low levels where the brain is deprived of glucose, signs and symptoms become progressively worse."
Time matters. What starts as mild shakiness can quickly progress to confusion, seizures, or even coma if left untreated. The good news? Most episodes can be resolved in 15 minutes with the right treatment.
Key sign of low sugar in the body vocabulary:
The Spectrum of Symptoms: Recognizing a Sign of Low Sugar in the Body
Your body has an early warning system for dropping blood sugar, but symptoms can vary between people and episodes. Recognizing the signs as they progress is key to preventing a serious event.
Early & Mild Warning Signs
When blood sugar dips, your body releases adrenaline, causing the first line of defense. The most common early sign of low sugar in the body is shakiness or trembling, often paired with sudden, clammy sweating. Your heart might start racing or pounding, triggering feelings of anxiety or nervousness.
Irritability is another telltale sign, as your brain lacks the fuel to regulate emotions. You may also experience intense hunger, nausea, dizziness, chills, and paleness. For people with diabetes, these signs often appear when glucose drops to around 70 mg/dL. The nausea can be especially challenging, as detailed in our guide on blood sugar drop nausea.

Worsening Signs as Blood Sugar Drops
If early signs are missed, your brain starts to malfunction from the lack of glucose. Confusion and difficulty concentrating are major concerns, making simple tasks feel overwhelming. You may also experience blurred vision or slurred speech.
Physical coordination breaks down, leading to clumsiness and a lack of coordination. Despite earlier anxiety, profound drowsiness or fatigue can set in, along with headaches. Perhaps most concerning is unusual behavior, such as aggression or withdrawal, that is out of character. These symptoms typically indicate blood sugar has dropped below 55 mg/dL, requiring immediate action.
Signs of Severe Hypoglycemia: A Medical Emergency
Severe hypoglycemia is a life-threatening medical emergency. The brain is so deprived of glucose that normal function shuts down, risking permanent damage or death.
| Symptom Category | Mild Hypoglycemia (Blood Sugar ~70 mg/dL) | Severe Hypoglycemia (Blood Sugar <54 mg/dL) |
|---|---|---|
| Physical | Shakiness, sweating, fast heartbeat, hunger, nausea, dizziness, paleness | Muscle weakness, inability to eat/drink, loss of coordination, unresponsiveness |
| Cognitive/Behavioral | Anxiety, nervousness, irritability, difficulty concentrating, mild confusion | Severe confusion, disorientation, bizarre behavior, slurred speech, seizures, loss of consciousness, coma |
The most alarming signs include seizures or convulsions and loss of consciousness or coma. The person may be unable to eat or drink and experience such severe muscle weakness that they become limp.
If you witness these symptoms, call 911 immediately. Never try to give an unconscious person food or drink. If glucagon is available and you know how to use it, administer it and place the person in the recovery position while waiting for help. Understanding this progression from a mild sign of low sugar in the body to a medical emergency is vital.
Special Cases: When the Signs Aren't Obvious
Not everyone experiences the typical sign of low sugar in the body. Sometimes, symptoms can be subtle, happen during sleep, or not appear at all.
Nocturnal Hypoglycemia: Signs of Low Blood Sugar While You Sleep
Nocturnal hypoglycemia occurs when your blood sugar drops while you sleep, often due to daytime activity, exercise near bedtime, or medication. You might be unaware until morning. Clues that it occurred include:
- Waking up tired or groggy despite a full night's sleep.
- Morning headaches.
- Nightmares or restless sleep.
- Damp sheets from heavy sweating.
If you suspect nighttime lows, talk to your doctor. They may suggest checking your blood sugar between 3 AM and 4 AM or having a bedtime snack.
What is Hypoglycemia Unawareness?
Hypoglycemia unawareness is a condition where you no longer feel the typical warning signs of low blood sugar. It often develops in people with long-term diabetes or those who experience frequent lows, as the body stops releasing the stress hormones that cause symptoms like shakiness and sweating.
The danger is that you might not realize your blood sugar is critically low until you experience severe symptoms like confusion or loss of consciousness. Regular monitoring is crucial for anyone with this condition. A continuous glucose monitor (CGM) is especially valuable, acting as a backup alarm system. More info about continuous glucose monitoring services can explain how these devices can help. Fortunately, it's sometimes possible to regain your ability to feel lows by strictly avoiding them for several weeks.
What if I feel a sign of low sugar in the body, but my levels are normal?
Sometimes you may feel symptoms of a low, but your glucose meter shows a normal or high reading. This is known as pseudo-hypoglycemia. It can happen if your glucose drops quickly from a very high level (e.g., from 300 mg/dL to 150 mg/dL). Your body reacts to the rapid drop, not the absolute number. It can also occur when your body is adjusting to healthier A1C levels after a period of prolonged high blood sugar.
The key is to trust your meter, not just your feelings. If your reading is normal or high, do not treat with carbohydrates, as this could cause your glucose to spike. Instead, consult your doctor to understand why these episodes are happening and adjust your management plan. The importance of testing is the only way to know if a sign of low sugar in the body is real or your body adjusting to change.
What Causes These Symptoms to Appear?
Understanding why your body sends out these warning signals is key to prevention. The causes of a sign of low sugar in the body vary depending on whether or not you have diabetes.
Common Causes for People with Diabetes
For people with diabetes, managing blood sugar is a delicate balance. One study found that 4 in 5 people with Type 1 and nearly half with Type 2 on insulin experience a low over a four-week period. Common causes include:
- Too much insulin or diabetes medication: An incorrect dose, especially of insulin or oral drugs like sulfonylureas, is a frequent cause.
- Skipped or delayed meals: Medication continues to work even if you don't eat on time, causing glucose levels to fall.
- Increased exercise: Physical activity makes muscles use glucose more efficiently, which can lead to lows if you don't adjust food or medication.
- Alcohol consumption: Alcohol interferes with the liver's ability to release stored glucose, an effect that can occur hours after drinking.
- Other factors: Schedule changes, travel, hot weather (which can speed up insulin absorption), and hormonal fluctuations can all disrupt blood sugar control.
Causes for People Without Diabetes
While less common, hypoglycemia in people without diabetes often points to an underlying health issue.
- Reactive hypoglycemia: This occurs within a few hours after a meal, particularly one high in simple carbs, when the pancreas overreacts and releases too much insulin. It's more common in people who are overweight or have had gastric bypass surgery.
- Fasting hypoglycemia: This happens after long periods without food and can have more serious causes, such as binge drinking on an empty stomach.
- Certain medications: Drugs for other conditions, like quinine or some antibiotics, can cause low blood sugar as a side effect.
- Severe illnesses: Conditions like severe liver disease, kidney failure, or sepsis can impair the body's glucose regulation.
- Hormone deficiencies: Problems with the adrenal or pituitary glands (e.g., Addison's disease) can affect hormones crucial for maintaining blood sugar.
- Pancreatic tumors (insulinomas): In rare cases, these tumors produce excess insulin, leading to frequent lows.
If you experience symptoms without having diabetes, see a healthcare professional to identify the cause. For more details, scientific research on non-diabetic hypoglycemia offers comprehensive information.
How to Respond When You Spot the Signs
Recognizing a sign of low sugar in the body is the first step; knowing how to act quickly can prevent a mild episode from becoming an emergency.
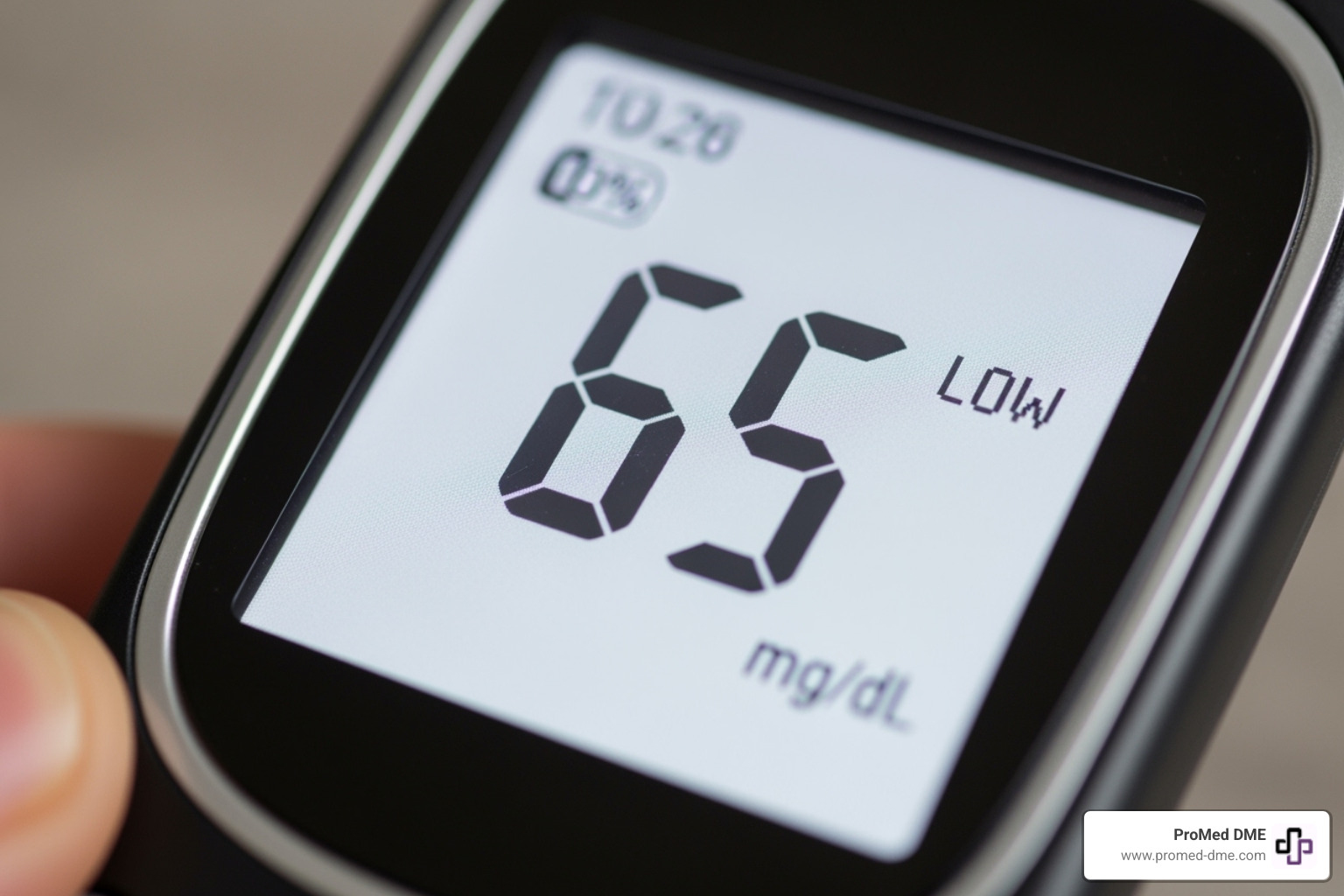
Step 1: Confirm with a Blood Sugar Test
The first thing to do when you suspect a low is to test your blood sugar. Your symptoms might feel like a low, but only a meter or CGM can confirm it. Stress or a rapid drop from a high level can mimic low symptoms.
The "when in doubt, treat" principle: If you have symptoms but cannot check your blood sugar immediately, it is safer to treat for a low. A temporary high from unnecessary treatment is far less dangerous than an untreated low. Keep a log of your levels, symptoms, and treatments to help your healthcare team identify patterns.
Step 2: Follow the 15-15 Rule for Treatment
Once you confirm your blood sugar is low (generally below 70 mg/dL), use the "15-15 Rule." This simple, effective method helps prevent over-treating.
1. Consume 15 grams of fast-acting carbohydrates. These are simple sugars your body can absorb quickly. Good options include:
- 3-4 glucose tablets
- Half a cup (4 oz) of fruit juice or regular soda (not diet)
- 1 tablespoon of honey or maple syrup
- 5-6 hard candies or jelly beans
Avoid chocolate or fatty foods, as fat slows down sugar absorption.

2. Wait 15 minutes. This is crucial. Your body needs time to absorb the sugar.
3. Recheck your blood sugar. If it's still below 70 mg/dL, repeat the process. Once your level is back in range, have a small snack with protein and complex carbs (like crackers with cheese) if your next meal is more than an hour away to stabilize your blood sugar.
Note for parents: Infants and small children may need smaller amounts of carbohydrates (8-10 grams). Always consult your child's care team for specific guidance.
Step 3: When to Seek Immediate Medical Help
Most lows are manageable, but some situations require immediate emergency medical attention. Call 911 immediately if the person:
- Is unconscious or unresponsive.
- Is having a seizure or convulsions.
- Is unable to swallow safely.
- Does not improve within 5-15 minutes after a glucagon injection.
Glucagon is an emergency hormone that rapidly raises blood sugar. If the person has a prescribed kit and you know how to use it, administer it immediately. While waiting for help, roll an unconscious person onto their side into the recovery position to prevent choking. Never give an unconscious person anything by mouth.
Ensure family and friends know the signs of a low, where your glucagon is, and how to use it. Wearing a medical ID bracelet can be life-saving.
Preventing Future Episodes and Staying Safe
The best way to handle a sign of low sugar in the body is to prevent it. This involves building sustainable habits to reduce the frequency and severity of low blood sugar episodes.
The Role of Consistent Monitoring and Diet
Your blood sugar responds to diet, exercise, sleep, and stress. Understanding these patterns is key to prevention.
- Regular blood sugar checks provide valuable data about your body's responses. A continuous glucose monitor (CGM) is especially crucial if you have hypoglycemia unawareness.
- Eat balanced meals that include protein, healthy fats, and complex carbohydrates to promote a steadier release of energy.
- Don't skip meals. Your body needs a consistent fuel supply to keep blood sugar stable. Keep healthy snacks on hand for long stretches between meals.
- Adjust for exercise. Physical activity can lower blood sugar. Discuss your routine with your healthcare team to learn how to adjust food or medication. Check your blood sugar before and possibly during workouts.
- Drink alcohol thoughtfully. If you drink, do so in moderation and always with food, as it can cause delayed hypoglycemia.
Special Considerations for Driving
Driving with diabetes requires extra vigilance to ensure your safety and the safety of others.
- Check your blood sugar before every drive. If it's below your target (e.g., 70 mg/dL), treat the low and wait to drive.
- On long trips, pull over safely every two hours to recheck your levels.
- If you feel any sign of low sugar in the body while driving, pull over immediately and treat it.
- Wait at least 45 minutes after your blood sugar returns to normal before driving again. This allows your brain's cognitive function to fully recover.
- Always keep fast-acting carbohydrates within easy reach in your car.
In some regions, you may be legally required to stop driving and inform the licensing authority if you have multiple severe hypoglycemic episodes. For example, the DVLA has more information about hypoglycaemia and driving for UK drivers.
Frequently Asked Questions about Low Blood Sugar Signs
Here are answers to some of the most common questions about recognizing and managing a sign of low sugar in the body.
What's the difference between hypoglycemia and hyperglycemia?
The prefixes "hypo" (under) and "hyper" (above) help distinguish these opposite conditions.
- Hypoglycemia is low blood sugar (typically under 70 mg/dL). Symptoms include shakiness, sweating, and confusion. It requires immediate intake of sugar.
- Hyperglycemia is high blood sugar (often above 180 mg/dL). Symptoms include increased thirst, frequent urination, and fatigue. Treatment involves insulin or other measures as directed by a doctor.
Knowing the difference is critical for proper treatment.
How quickly do signs of low blood sugar appear?
Symptoms can appear very quickly, often within minutes of blood sugar levels starting to drop. However, the timing varies. Some people feel symptoms immediately, while those with hypoglycemia unawareness may not notice them until levels are dangerously low. A rapid drop in blood sugar, even from a high level, can also trigger symptoms faster than a gradual decline. The key is to recognize the signs as soon as they appear and act without delay.
Can stress cause low blood sugar symptoms?
Stress can mimic low blood sugar symptoms, but it typically raises blood sugar, not lowers it. During stress, your body releases hormones like adrenaline and cortisol, which signal your liver to release glucose. This "fight or flight" response can cause shakiness, a racing heart, and sweating—sensations very similar to hypoglycemia.
Because the symptoms are so alike, it's crucial to test your blood sugar. If your reading is normal or high, you'll know you're dealing with stress and should focus on management techniques rather than consuming sugar.
Conclusion: Taking Control of Your Blood Sugar Health
Recognizing a sign of low sugar in the body is about empowering yourself to live confidently. Understanding the progression from mild warnings like shakiness to severe symptoms allows you to act decisively.
The real power lies in proactive prevention. While knowing the 15-15 Rule is vital for treatment, the ultimate goal is to prevent lows through consistent monitoring, balanced eating, and understanding your personal triggers.
This journey can feel complex, which is why partnering with your healthcare team is so important. They can help you fine-tune your management plan. Having reliable tools is also key.
At ProMed DME, we understand that the right monitoring equipment can transform your confidence. Based in Stuart, Florida, we ship nationwide and are committed to providing top-quality supplies with exceptional service. With free shipping, a dedicated nurse on staff, and support for most insurance plans, we help you access the tools you need.
Your journey is unique. Stay vigilant, be prepared, and never hesitate to seek help. With the right knowledge and support, you can control your blood sugar, not the other way around. Learn more about how Continuous Glucose Monitoring can help you stay in control and provide peace of mind.
Related Resources & Articles
Stay informed with our informative blog posts.
Discover the ProMed Advantage
& Try Our Products
We offer free shipping and legendary customer service to ensure you receive the
best DME products for your needs.



